Osteoporosis is one of the most urgent challenges to people living well in later life. Over 200 million women suffer from osteoporosis, and it affects half of the women over the age of 50. Women are particularly susceptible because of the rapid bone loss that occurs at menopause. Once identified, osteoporosis is treatable. Treatments for osteoporosis have been shown to be effective in increasing bone strength and substantially reducing fracture risk. Despite having effective fracture risk assessment tools and treatments, currently, only a minority of people who need osteoporosis treatment are receiving it. This is called the ‘treatment gap’ and is well recognized. In 2019, 66% of people in the UK who were at high risk of fracture had not received treatment.
Osteoporosis has an image problem. It has been reported as ‘not being a sexy subject, it happens to older women, it is an inevitable part of aging.’ Why are we neglecting to assess, diagnose and treat so many women? An assessment of risk for osteoporosis takes less than one minute, and without a doubt could save a life.
The effects of osteoporosis vary considerably. Some people have no fractures and therefore no symptoms at all. Some people have fractures and fully recover. Others may have long-lasting effects from fractures such as difficulty walking, pain, or needing help with daily activities.
50% of postmenopausal women are currently expected to have a fragility fracture in their lifetime. One in six women will have a hip fracture and, of these, 20% will die within a month and 30% within a year. The annual number of hip fractures in the UK due to osteoporosis has risen by 44% since 2006 with numbers now greater than 100,000. Spinal fractures are associated with significant back pain and poor quality of life.
Any postmenopausal woman, who has not had a fracture, but who has a clinical risk factor for osteoporosis should have a FRAX assessment. Any postmenopausal woman with a previous fragility fracture should be considered for treatment or osteoporosis without the need for further risk assessment, although measuring bone mineral density may be appropriate.
The Living Skeleton
Bones are alive and they change throughout life. They are made up of a matrix of proteins and minerals, making them both strong and flexible. They contain osteocytes, which are cells that maintain bone matrix. Older bone tissue is broken down (resorbed) by cells called osteoclasts, and new bone is rebuilt by cells called osteoblasts. This is described as bone remodelling. Until the age of 45, there is usually a balance between the amount of bone removed and created, so the amount of bone tissue remains stable. After menopause, due to the declining sex hormone changes, bone resorption (breakdown) exceeds bone formation which leads to a rapid decline in bone mass.
How does oestrogen affect bone metabolism?
Oestrogen is the major hormonal regulator of bone metabolism in women, it is a sex hormone that is essential to female bone health.
Experts do not understand exactly how oestrogen affects bone, but they believe that the complex relationship between the two involves:
The Immune System
Oestrogen may affect bone homeostasis by regulating the immune system.
Effects on Bone Cells
Oestrogen influences osteocytes, as well as osteoblasts and osteoclasts. Oestrogen maintains bone mass by decreasing the lifespan of osteoclasts and increasing osteoblast and osteocyte survival.
Oxidative Stress
Oxidative stress alters the bone remodelling process causing an unbalance between osteoclast and osteoblast activity. Oestrogen also may affect bone health via its effect as an antioxidant to protect the bone against oxidative stress.
Sema 3A Protein
There may be a relationship between oestrogen and the sema3A protein in osteocytes. As people age, their levels of oestrogen and sema3A deplete, which leaves the bones unable to maintain their structure.
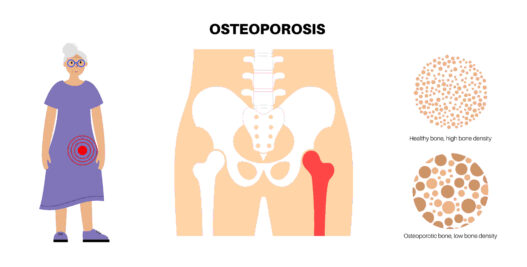
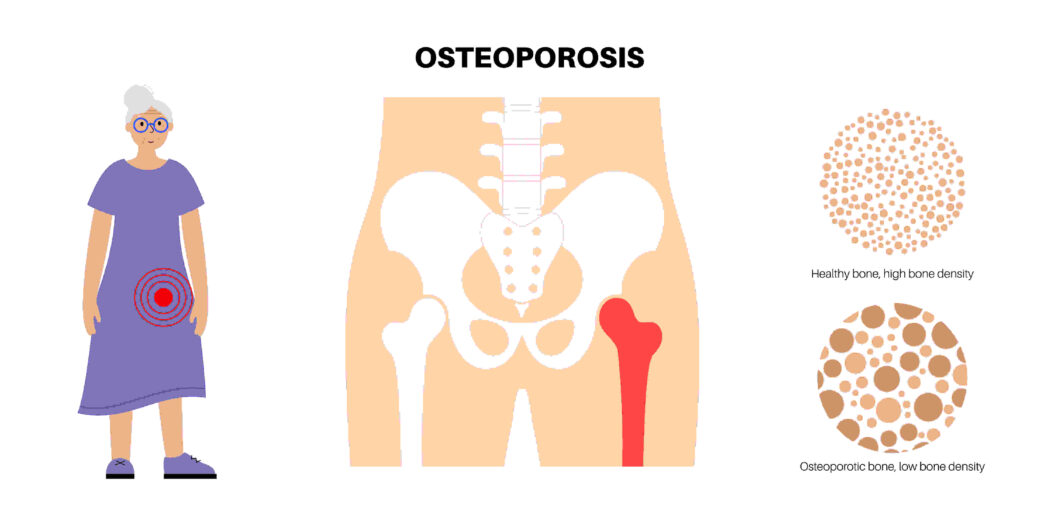
What is Osteoporosis?
Osteoporosis is a chronic bone disease characterized by low bone mass and deterioration of bone tissue. This means bones are more likely to break when we have no injury or a minor bump or fall from standing height or less. A break like this is called a fragility fracture.
The World Health Organization (WHO) defines osteoporosis using a T-score, which is a measure of bone density compared to average healthy women in their 20s. Osteoporosis is defined as a T-score of -2.5 or less.
Osteoporotic fractures commonly occur at the wrist, spine, and hip. These types of fractures have a huge impact on quality of life, they result in an economic burden and are associated with increased mortality.
What are the clinical risk factors for osteoporosis?
Some of the clinical risk factors for osteoporosis and/or a fragility fracture that would trigger a FRAX assessment include:
- A previous fragility fracture,
- A fall,
- Use of glucocorticoids,
- A low BMI < 18.5kg/m2 or previous anorexia,
- Parental history of hip fracture,
- Rheumatoid arthritis,
- Alcohol ≥3U/day,
- Current smoking,
- Diabetes (either type),
- Frailty,
- Thoracic kyphosis,
- Height loss >4cm,
- Chronic malabsorption and bariatric surgery,
- Chronic lung, liver, muscle, renal, neurological or inflammatory disease, HIV, malignancy, primary hyperthyroidism, hyperparathyroidism, hypogonadism,
- Early menopause (before 45 years),
- Use of aromatase inhibitors and androgen deprivation therapy. This list is not exhaustive, and drugs known to decrease bone mineral density also include proton pump inhibitors, SSRIs, anticonvulsants, and diabetic medications called thiazolidinediones.
FRAX
The FRAX (Centre for Metabolic Bone Diseases, University of Sheffield) is an online calculator validated for patients aged 40-90 years. FRAX calculates the patient’s 10-year risk of hip and major osteoporotic fracture, and links to the National Osteoporosis Guideline Group (NOGG) which advises further action. This could be with either lifestyle advice, and reassessment in 5 years or sooner; a bone density scan, or advice to start treatment for osteoporosis, without the need for a bone density scan.
A Bone Density Scan
DEXA scan stands for dual-energy X-ray absorptiometry. It’s also called a bone densitometry scan. It uses low-dose X-rays to take measurements to work out the strength (density) of bones.
When to start treatment, if osteoporosis is diagnosed?
If osteoporosis is diagnosed, it is important to start treatment as soon as possible after a fragility fracture as the risk of having another fracture is highest immediately after the first fracture; this increase in risk remains particularly high for up to 2 years.
Treatment of Osteoporosis
Women who are diagnosed with osteoporosis have a selection of treatments available, oestrogen and non-oestrogen based, the choice should be targeted to the needs of the individual woman.
Hormone replacement therapy (HRT) has been shown to be effective in preserving bone density and in reducing the risk of spine, hip, and other osteoporotic fractures in women over 50 years and should be considered the first-line therapeutic intervention for the prevention and treatment of osteoporosis in women with premature ovarian insufficiency (POI) and symptomatic women below 60 years of age (BMS).
Women who have experienced early menopause (whether natural or surgically induced) should be recommended HRT until at least the normal age of menopause (around 50 years).
For postmenopausal women below the age of 60, HRT can be considered as first-line treatment for osteoporosis, providing that the beneficial effects on fracture risk reduction outweighs any adverse risks for that individual (BMS).
Initiating HRT after the age of 60 years for the sole purpose of prevention of osteoporotic fractures is not recommended by the BMS, but it should be considered for osteoporosis prevention in women over the age of 60, who continue to benefit from HRT in terms of menopause symptom relief.
Interventions for the prevention and treatment of osteoporosis
- Hormone replacement therapy
- Bisphosphonates such as Alendronate, Risedronate, Ibandronate, and Zoledronate
- Denosumab
- Raloxifene
- Parathyroid hormone peptides
- Romozosumab
- Calcium and Vitamin D
- Exercise
Lifestyle advice
Lifestyle advice to women should include eating a healthy, well-balanced diet with the right daily intake of calcium and vitamin D, doing regular weight-bearing and muscle-strengthening exercises, advice not to smoke, limiting alcohol intake, and taking measures to reduce their risk of falling over.
Women with osteoporosis, or who are at high risk of developing osteoporosis, need lifelong management and we must check every postmenopausal woman for risk factors and assess her risk of fracture.
Support Leaflets for Women
Sources
https://www.nogg.org.uk/resource-centre. Post reproductive health 2023 Vol 29(1) 11-14.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3424385
https://www.endocrineweb.com/conditions/osteoporosis/estrogen-replacement-therapy-osteoporosis
https://www.medicalnewstoday.com/articles/estrogen-and-osteoporosis#low-estrogen-levels
https://www.eurekaselect.com/article/107105
Lean JM, Jagger CJ, Kirstein B, Fuller K, Chambers TJ. Hydrogen peroxide is essential for estrogen-deficiency bone loss and osteoclast formation. Endocrinology. 2005;146:728–735.
Manolagas SC. From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev. 2010;31:266–300.
Baek KH, Oh KW, Lee WY, Lee SS, Kim MK, Kwon HS, Rhee EJ, Han JH, Song KH, Cha BY, Lee KW, Kang MI. Association of oxidative stress with postmenopausal osteoporosis and the effects of hydrogen peroxide on osteoclast formation in human bone marrow cell cultures. Calcif Tissue Int. 2010;87:226–235.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3424385
https://www.sciencedirect.com/science/article/pii/S1550413118307587
https://www.sciencedaily.com/releases/2019/03/190322105728.htm.

Dr. Carys Sonnenberg is an NHS GP with a special interest in Women’s Health and Menopause. She runs an NHS women’s health clinic at her practice. She is a British Menopause Society trained doctor and is completing the advanced menopause training to become a BMS Menopause Specialist. She is the founder of Rowena Health, which she runs, and enables her to offer private appointments to women for holistic menopause care, all over the UK. She is passionate about education and sits on the Education Committee for the Primary Care Women’s Health Forum. In her free time she loves walking her dog and spending time outdoors with family and friends.