Ah, midlife—the time when men swap their sports cars for sedans, beers for green teas, and hair for a shiny new scalp. Welcome to the curious and comical world of MANopause, the lesser-known, testosterone-tumbling sibling of menopause and male aging. If you’re a man in your 40s or 50s—or if you live with one—buckle up for a journey through the hilariously relatable pitfalls of this male midlife mystery. Manopause or Male menopause or Andropause or late-onset hypogonadism, is a condition in males over 40 where they have significantly lower testosterone levels, causing many problems like low libido, depression, etc.
This topic is not often talked about or is often confused with female menopause. In this article, we will learn more about male menopause and the basic differences between female and male menopause i.e. Manopause vs Menopause, understand the symptoms, and, in the end, try to find solutions, if any. But first, we need to learn what testosterone is and how low levels can create absolute wreckage.
What is testosterone and how it could fall?
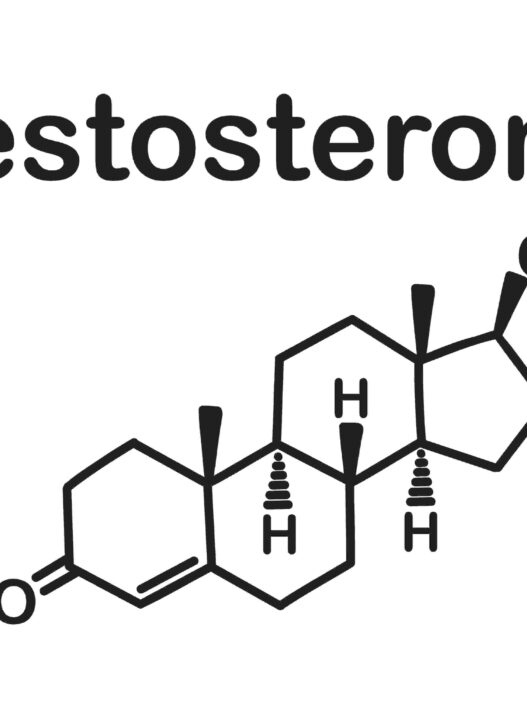
Testosterone (1) is the main male sex hormone or steroid hormone. It is often associated with masculinity; however, it is present in both men and women (in very small quantities).
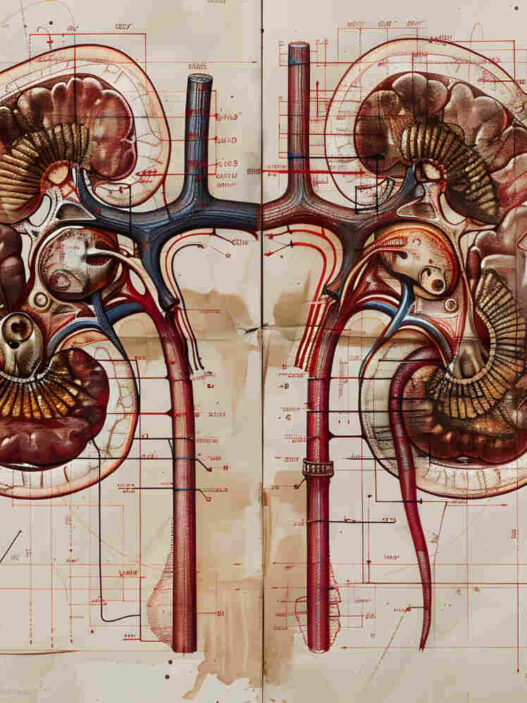
This hormone is produced primarily in men’s testicles and also in the adrenal glands (in small quantities). There are many functions that testosterone plays in men.
Its main role is the development of the male sex organs during puberty. It also determines sperm production, libido (sex drive), and erectile function. Other than that, it plays a major role in the development of muscle mass growth and strength and in maintaining bone density.
Testosterone also stimulates mood and energy. It gives a feeling of confidence, motivation, and stamina.
So, you can see how important testosterone is and how significant disturbances can occur if its levels are low.
The body may need testosterone for various functions, and sex hormone-binding globulin (SHBG) plays a role in this. SHBG binds testosterone and other sex hormones to the bloodstream. Testosterone that is not bound to the bloodstream is called bioavailable testosterone, and it interacts with cells and plays a major role overall.
MANopause vs Menopause – Difference between male menopause and female menopause
The female menopause and male menopause are two conditions that are often confused and not talked about openly. A lot of people don’t know about them especially MANopause, the male menopause and even consider them taboo subjects. So lets compare Manopause vs Menopause and understand how these conditions differ.
Female menopause, or simply menopause, occurs after the age of 51. This, in simple terms, means a permanent end to menstruation and fertility. Women are born with a finite number of eggs. When these eggs are depleted and ovulation stops, it leads to a decline in hormone production like estrogen.
This means the end of fertility completely. In some cases, women may experience early menopause. This could be due to surgery, autoimmune disease, chemotherapy, genetics, etc.
For detailed understanding of menopause, please refer to our Women’s health page for the detailed discussion, awareness, symptoms and myth busters by menopause physicians – Dr. Carys Sonnenberg, NHS GP and British Menopause Society trained physician and Dr. Vikram Talaulikar, MD, a Specialist in Reproductive Medicine at University College London Hospitals NHS Foundation Trust.
Male menopause typically occurs between the ages of 40 and 55 but starts as early as 30 years of age, where males experience a decline in testosterone production. However, it doesn’t mean a complete end of fertility. That’s an important distinction between Manopause vs Menopause.
Unlike women, who most often experience menopause after 50, males can experience it immediately after 30, and there are various reasons for that.
Additionally, the testosterone levels decline slowly and gradually, roughly 1% per year after the age of 30 unlike women where there is abrupt hormonal drop experienced during menopause.
Reason and risk factors of Manopause/ Andropause
Now we know the difference Manopause vs Menopause, let us understand the risk factors for MANopause. Andropause, also referred to as late-onset hypogonadism, means a gradual decrease in testosterone leading to male menopause or Manopause. Please note, “gradual” is an important word here, because testosterone doesn’t magically decrease in one day (remember Manopause vs Menopause).
Some reasons are:
Aging
With age, testosterone starts decreasing (1% every year after 30), and in some cases, it is noticeable because it can lead to a decrease in sex drive or erectile dysfunction. In other cases, men may not realize it.
Poor Diet
Food influences testosterone production. A diet rich in sugar and refined carbs can lead to insulin resistance, which can disrupt hormone production in the entire body, including testosterone.
Similarly, processed food and fried food are linked (2) with impaired testosterone signaling and testicular function.
Additionally, a diet that lacks zinc, vitamin D, or magnesium can also hinder testosterone synthesis.
Lack of Exercise
Exercise boosts testosterone. We need to understand that with age, testosterone will decline, so even if one doesn’t engage in any form of physical activity, testosterone will gradually decline. However, no physical activity will accelerate this decline further.
A sedentary lifestyle and a diet high in trans-fat and sugar often lead to obesity. Obesity is linked (3) to low testosterone production and more estrogen production, leading to conditions like “man boobs,” etc.
Stress
Stress is also one of the reasons for significantly low testosterone production. High cortisol levels can suppress testosterone because the body is more concerned with dealing with stress and less with hormonal function.
There is research (4) that suggest that high level of cortisol can suppress testosterone production. Study revealed that even short term acute stress can decrease testosterone in healthy young men.
Substance Abuse
Excess always harms, and smoking, alcohol, and many drugs affect testosterone production.
Certain steroids are often taken to mimic testosterone function in relation to muscle growth, but they badly suppress natural testosterone production.
Long-term tobacco use and smoking are linked (5) to lower testosterone levels according to some studies.
Alcohol damages the Leydig cells in the testes, which are responsible for testosterone production. Leydig cells are specialized cell that synthesize testosterone through a serious of biochemical function. It can also get damaged due to age, medication, environmental toxins, stress and traumas.
Other Reasons
There are several other factors that are not much discussed, such as medication or testicular injury, which may be reasons for andropause. These could lead to a decline in testosterone at an early age.
Family history may also influence the timing and severity of andropause.
Studies (6) have shown that sunlight and testosterone are closely related. In simple terms, sunlight regulates circadian rhythm, which is linked to hormonal production. Studies have also connected how an increase in sunlight can lead to a modest boost in testosterone.
We have already discussed how insulin resistance and obesity could be reasons, and adding sleep apnea and cardiovascular diseases to that as well. These factors may not seem directly related to testosterone production, but many studies have shown us how they influence this relationship.
MANopause or Andropause: Symptoms
Unlike female menopause, which generally occurs at a certain age, MANopause, the male menopause or andropause can occur at any age (the above-mentioned reasons exacerbate it further).
These symptoms may vary from person to person, and it’s not necessary that everyone will experience them:
- Low sex drive and lack of desire
- Lack of energy
- Depression (testosterone is not the only reason)
- Difficulty in getting erections
- Loss of strength and muscle mass
- Height loss or effects on growth
- Chest discomfort
- Hair loss
- Low mineral density
- Increased body fat
- Gynecomastia
- Insomnia or difficulty sleeping
The hormonal changes that occur in Male menopause can lead to several physical changes leading to above symptoms. An increase in body fat, particularly around the abdomen, and a decrease in muscle mass and strength is also commonly observed. Men with andropause or MANopause are more susceptible to fractures and osteoporosis because of decreased bone mineral density or BMD.
Manopause doesn’t just cause the physical health; it has significant emotional and cognitive consequences. Thus, symptoms such as fatigue, depression, irritability, and difficulty concentrating are commonly reported attributed to low testosterone levels. The symptoms of depression are exhibited mainly as Anhedonia (inability to derive pleasure from usually pleasurable activities), lack of energy and exhaustion and cognitive impairment (11).
Some studies have shown that a decline in testosterone can lead to cardiovascular disease, increased LDL cholesterol, and inflammation. Thus, high blood pressure, high blood sugar, excess fat around the waist, and abnormal cholesterol levels during Manopause have all been linked to increased risk of heart disease, stroke, and type 2 diabetes. Testosterone decline is also associated with reduced libido, erectile dysfunction and sexual performance issues. Addressing these symptoms often involves a multifaceted approach, incorporating lifestyle changes, counselling, and possibly testosterone replacement therapy or TRT, as discussed in the following section. However, TRT is only recommended under medical supervision and advise.
For understanding the differences of symptoms with respect to Menopause vs Menopause, please check out Menopause symptoms here.
MANopause: Diagnosis and treatment
Levels of testosterone can be determined through a normal blood test, but for treatment, one must consult a doctor. Understanding male menopause on a personal level can be challenging, hence consulting a doctor is crucial. Only a doctor can guide the right or easy step, hence don’t try to find ways online and see a doctor.
If a person is diagnosed with late-onset hypogonadism, treatment may involve hormonal replacement therapy where additional testosterone is provided as needed.
Last year, The East Midlands Ambulance Service made headlines by reportedly granting 1 year of paid leave to men experiencing andropause. However, this decision sparked controversy, questioning the legitimacy of andropause.
Lifestyle changes are essential in managing andropause. As discussed, a diet high in sugar, processed food, and trans fats is harmful to testosterone levels, whereas a diet rich in fruits, fresh veggies, legumes, and lean proteins is beneficial. The same is also true for menopause when comparing Manopause vs Menopause.
Healthy fats such as fatty fish, olive oil, seeds, and nuts can positively impact testosterone levels. A healthy diet also provides important nutrients like Vitamin D, zinc, and magnesium.
Research (7) has shown that men with vitamin D deficiency who received supplements for a year experienced a significant increase in testosterone levels.
Similarly, zinc is crucial for testosterone production in the testes. Several studies (8) have demonstrated a relationship between lower zinc levels and low testosterone levels.
Evidence regarding magnesium’s direct impact on testosterone production is limited, but combined with zinc supplements, it has shown some positive outcomes on testosterone levels.
Certain forms of exercise are considered beneficial (9) for boosting testosterone. Significant increases in testosterone levels have been observed immediately after a workout (short-term) and with consistent exercise.
A healthy diet and regular exercise can naturally boost testosterone levels. Combining a balanced diet with adequate sleep is essential for optimal testosterone production.
Resistance training (or strength training) is widely regarded as the most effective (10) way to boost testosterone, as it challenges muscles and stimulates hormone release.
HIIT (High-Intensity Interval Training) has also been found to temporarily elevate testosterone levels.
Any further medication should only be prescribed by a doctor and varies for each individual.
There is growing interest among young men in supplements that claim to boost testosterone. Many take these supplements without prescription in hopes of building muscle.
Popular ingredients in these supplements include Ashwagandha, Fenugreek, Shilajit, Tribulus Terrestris, etc. However, there is insufficient high-quality research to support their effectiveness in boosting testosterone.
While these ingredients may show promise in areas like stress reduction and improved mineral absorption, their effectiveness in boosting testosterone is not well-supported by current research.
In the end
MANopause needs more awareness. The NHS does not officially recognize menopause or andropause as a medical condition. Andropause can be treated if people are more open about their symptoms, at the right time.
Menopause, in general, is considered a taboo subject. Men’s and women’s health issues are still not openly discussed, and people are often reluctant to talk about them. Men are shy to see a doctor for such conversation. When they read stuff online, they get misguided and feel hopeless. However, as we stated at right time, treatment is possible.
A few strategies can help boost testosterone levels, but overall, a healthy lifestyle is key.
With that, we hope this article will serve as a quick reference on this important subject.
Sources
- https://www.nih.gov/news-events/nih-research-matters/understanding-how-testosterone-affects-men
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6660671/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3955331/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9653469/
- https://pubmed.ncbi.nlm.nih.gov/17163954/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7241626/
- https://pubmed.ncbi.nlm.nih.gov/32446600/
- https://pubmed.ncbi.nlm.nih.gov/36577241/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5924956/
- https://pubmed.ncbi.nlm.nih.gov/21058750/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4440190/