Menopause and Insulin Resistance, what can we do? Diet for insulin resistance? Exercise? HRT? Why does menopause increase the risk of type 2 diabetes?
Menopause and Insulin Resistance – What can we do?
The Questions – Diet for insulin resistance? Exercise? HRT?
High GI or Low GI foods?
Insulin? What is it?
Why shouldn’t I just tuck into a bowl of pasta?
Why worry about menopause and insulin resistance? Does diet help?
What does it all mean for my menopause?
Does HRT help?
It can be confusing!
What does glycemic index mean?
After a meal or snack, carbohydrates are broken down in the digestive tract and changed into glucose. Glucose is then absorbed into the bloodstream through the lining of the small intestine.
Glucose is our fuel, our cells use it to make energy for the body. Remember learning about the Krebs cycle in the mitochondria of cells, releasing energy from glucose, to be used by the cell?
Carbohydrates are not all the same.
The glycemic index (GI) rates carbohydrates from 0-100 based on how quickly they release glucose into our bodies. Do we want a fast rise or a low rise in blood sugar? Yes, a slow steady rise is safer, it keeps our blood sugar stable. Does it matter if our blood sugar is high? Yes, it increases the risk of Type 2 Diabetes.
High GI carbohydrates, such as pasta, bread, rice, processed foods, sugary drinks, fast food, sweets, and cakes, have a GI number over 70, these are high glycemic index foods. The consequence of eating these foods is a rapid release of glucose into the bloodstream, a surge in blood glucose, followed by a rapid fall in blood glucose, leaving you tired and hungry quickly.
Eating food with a high GI index is linked to an increased risk of Type 2 Diabetes, Cardiovascular disease, and Obesity. It is also linked with Age-Related Macular Degeneration and colorectal cancer.
Low GI carbohydrates, such as whole grain rice, vegetables, fruits, legumes, dairy products, and nuts give a lower and slower rise in blood sugar and have a GI number below 70. Replacing your high GI carbohydrates with low glycemic index ones will keep your blood sugars more stable and avoid high sugar spikes which lead to a surge in required insulin levels.
Studies show that eating foods with fat and fibre also causes a more gradual rise in blood sugar.
Why worry about high blood sugar and what is insulin?
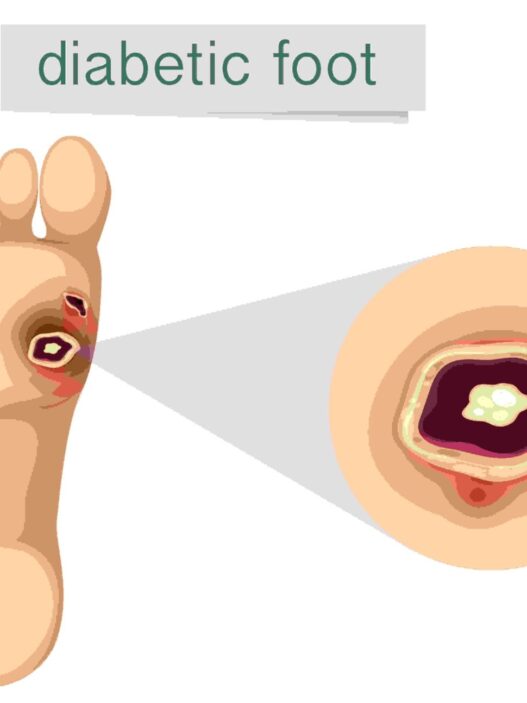
Having high blood sugar has been linked with Type 2 Diabetes, and diabetes-related complications including heart disease, stroke, and neuropathy. Menopause and insulin resistance is common.
Insulin
Insulin is a hormone released by the beta cells of the pancreas. It is a protein made up of 51 amino acids. Almost all the body’s cells have insulin receptors.
What does it do?

Insulin is the key that opens the cell glucose channel allowing glucose to enter the cell.
Insulin activates the rate of cellular respiration (glycolysis, pyruvate oxidation, the Krebs cycle and oxidative phosphorylation), so glucose is used to produce energy.
Insulin increases the rate of conversion of glucose into glycogen in the liver and muscles. If glucose cannot get into the cell, it is converted into glycogen by glycogenesis and this is stored in the liver and muscles to be converted back to glucose, at another time, when needed, to keep our blood sugar stable, for example, when we are fasting for hours.
The liver can store up to 100g of glycogen and this is changed back into glucose by Glycogenolysis. When Glycogen runs out, the body can make glucose from Gluconeogenesis, using non-carbohydrate sources like glycerol and amino acids. All to keep stable blood sugar.
Extra glucose, with the help of insulin, is converted into fatty acids and stored in adipose tissue, causing weight gain. If there is too much fatty acid, some of this builds up in the liver, causing a non-alcoholic fatty liver, which can lead to serious liver damage.
When blood sugar is consistently raised, it can lead to many chronic health conditions, including Cardiovascular Disease, Stroke, Type 2 Diabetes, Renal failure, Blindness, and Neuropathy. When insulin levels rise, it puts the brakes on burning fat for fuel, and it encourages the storage of incoming food, mostly as fat. If your diet is high in carbohydrates, the body never has a chance to burn its own fat, making weight loss difficult.
What is Insulin resistance?
Insulin is produced, in response to a rise in blood sugar, but cannot work properly, because the insulin receptors become insensitive or resistant, and don’t let the insulin open the gate in the cell to allow the glucose into the cell, to produce energy. Consequently, the cell cannot function correctly. High blood glucose levels result, high insulin levels result, and cells are starved of glucose.
Menopause and Insulin Resistance
The reduction of oestrogen in postmenopausal women accelerates the development of insulin resistance and type 2 diabetes. Estradiol has a positive influence on insulin sensitivity and beta-cell pancreatic function that could be lost after menopause.
Stress, which is common in menopause can increase insulin resistance and acute sleep deprivation, certainly common in menopause, has been reported to raise blood sugar. Insulin resistance increases with increasing body mass index, as we gain weight in menopause. Obesity, Type 2 Diabetes and metabolic syndrome, hypertension, PCOS, non-alcoholic fatty liver disease, and certain forms of cancer are associated with insulin resistance.
Menopause and Type 2 Diabetes
3.9 million people are now living in the UK with Type 2 diabetes, this figure is set to rise to a staggering 5.3 million by 2025, due to obesity and the natural effects of aging. Declining ovarian function is known to increase the risk of diabetes. Premature menopause increases the risk of diabetes by 32%.
Why does menopause increase insulin resistance and the risk of type 2 diabetes?
There are several physiological and metabolic reasons why ovarian function decline and low oestrogen levels increase weight gain and the risk of Type 2 diabetes.
- There is an increase in abdominal fat.
- Oestrogen deficiency favours fat storage and deposition, and there is reduced fat oxidation, the breakdown of fat to release energy.
- Women after menopause can be less active.
- Postmenopausal women have decreased muscle mass. Normal aging results in loss of muscle, known as sarcopenia.
- The pancreas gets tired, and the beta cells must work harder in women with insulin resistance. So, if there is a genetic predisposition to diabetes, there is a higher risk of this developing in the postmenopausal woman.
- Insulin resistance is compounded by increased chronic systemic inflammation. Visceral fat is an active tissue that secretes hormones and cytokines, this plus an androgen excess as happens when oestrogen levels fall in menopause, supports the development of insulin resistance.
How to reduce insulin resistance in menopause and your risk of chronic illness? Does HRT help?
Menopause and insulin resistance – how to reduce? HRT can reduce insulin resistance. There is very convincing evidence that supports the use of HRT in women with Type 2 Diabetes.
In a large meta-analysis, including 107 publications, HRT was shown to be statistically significant in:
- Reducing levels of abdominal fats.
- Improving insulin resistance.
- Reducing the incidence of new cases of T2DM.
- Reducing blood pressure.
- Favourably changing blood cholesterol, reducing the bad LDL cholesterol and improving the LDL/HDL ratio.
How HRT Works in Menopause and Insulin Resistance?
HRT works because:
Oestrogen reduces abdominal fat deposition, by increasing fat oxidation, and breaking fat down to produce energy.
Oestrogen acts directly on muscle, liver and fat cells reducing insulin resistance.
Oestrogen may also be able to act on the pancreas to stimulate insulin secretion.
The trials found that the most favourable results were with oral HRT.
Progestogens blunt the effect of oestrogen. Different progestogens have specific glucocorticoid (anti-inflammatory) and mineralocorticoid (regulation of salt and water) action, both of which can affect insulin resistance. Natural progesterone is felt to be the best. Utrogestan is a body identical progesterone, like the one made in our body.
We can see the evidence for using HRT in reducing insulin resistance. Replacing oestrogen using HRT has so many other health benefits.
- Reduction in Dementia, the number 1 cause of female death; this may be by increasing antioxidants; blocking some of the harmful effects of the Amyloid beta-protein which can cause damage to brain cells; by affecting our neurotransmitters in the brain or by affecting the area of the brain called the hippocampus, which is important for memory and learning.
- Reduction in cardiovascular disease if started early, within 10 years of menopause. Cardiovascular disease is the 3rd biggest killer of women.
- Reduction in osteoarthritis, as oestrogen is an anti-inflammatory.
- Reduction in Cognitive decline, as oestrogen modulates the neurotransmitters in the brain like serotonin, GABA and Glutamate.
- Reduction in osteoporosis, as oestrogen stimulates osteoclasts to make bone.
Oestrogen is so important to our bodies, these are only some of the ways in which it helps the female body. However, it is not the only way, as lifestyle is paramount in the fight to reduce insulin resistance and the progression to Type 2 Diabetes.
Aside from HRT, what can I do to reduce my risk of insulin resistance in menopause?
Insulin Resistance and Diet
Insulin Resistance and Menopause – Does diet help in insulin resistance? Women need to be advised to keep a BMI in the healthy range of 20-25. Being overweight increases your risk of Type 2 Diabetes, Heart Disease, and Stroke. Women should be eating a protein-rich, low-GI food diet to avoid high surges in blood glucose and avoiding insulin resistance.
Women should have a rainbow diet, full of nutrients, ensuring calcium intake is optimal at 1200mg a day (post-menopausal calcium requirements) and should consider Vitamin D supplementation to ensure bone health at 800IU a day. Diet is extremely important to manage insulin resistance in menopausal women. This dietary change does not need to wait until menopause, all through our lives our diet is vitally important to gain the correct nutrients from our food. Being overweight comes with so many health risks, increased risk of cancer, being another major risk.
Insulin Resistance and Exercise
Insulin Resistance and Menopause – Does exercise help in insulin resistance?

Exercise is also vital in addition to the diet. Exercise reduces insulin resistance.
The benefits of regular exercise seem endless, yet so many women struggle to fit it into our sedentary lifestyles. Time in the car, time at sitting work, time on our mobile phones, time watching television. Exercise shouldn’t wait till menopause, it should be a daily habit for us all, from childhood onwards. Life has become so busy, but we must make healthy choices, reduce insulin resistance, control weight, improve cognitive function, reduce the risk of osteoporosis, improve muscle tone, improve balance and therefore reduce the risk of falling and sustaining a fracture etc.
All adults should aim to do at least 150 minutes of moderate-intensity activity a week or 75 minutes of vigorous-intensity exercise over the course of a week. You can break this up into smaller manageable chunks, mix and match, and do what is fun, you’re much more likely to do it. If it’s a sociable exercise it will help with cognition, as will good sleep hygiene and cognitive exercises. It will help to reduce depression and anxiety.
There are so many benefits to being active. Walk instead of using the car, do a sport you enjoy, dance around the kitchen, it doesn’t have to be expensive, it just needs to get your heart rate up, get you hot and out of breath. It has huge benefits. So, can you eat that bowl of pasta? Well, the odd one is ok, but as we see our food choices, our diet, our exercise, and HRT will protect us from insulin resistance and many chronic health conditions that are now affecting our increasingly older population. It is our responsibility to step up and take action to reduce our risk of insulin resistance and Type 2 Diabetes.

Dr. Carys Sonnenberg is an NHS GP with a special interest in Women’s Health and Menopause. She runs an NHS women’s health clinic at her practice. She is a British Menopause Society trained doctor and is completing the advanced menopause training to become a BMS Menopause Specialist. She is the founder of Rowena Health, which she runs, and enables her to offer private appointments to women for holistic menopause care, all over the UK. She is passionate about education and sits on the Education Committee for the Primary Care Women’s Health Forum. In her free time she loves walking her dog and spending time outdoors with family and friends.