A holistic element of improving resistance, resilience, and recovery from long Covid through personalised nutrition and lifestyle interventions is described here highlighting five specific focus areas – Nutrition and Hydration, Microbiome Harmony, Metabolic Flexibility, Physical Fitness, and Mental well-being.
What is Long Covid?
Early on into the Covid-19 pandemic, it become clear that many people infected with the virus were experiencing symptoms long after the viral stages had passed. These symptoms have been collectively referred to as Long Covid. While there are some differences in definitions across health care authorities, NICE guidelines in the UK define long-term Covid patients as those with ongoing symptoms that persist beyond four weeks from the initial infection.
Official definitions from NICE
- Acute COVID-19 Signs and symptoms of COVID‑19 for up to 4 weeks.
- Ongoing symptomatic COVID-19 Signs and symptoms of COVID‑19 from 4 weeks up to 12 weeks.
- Post-COVID-19 syndrome Signs and symptoms that develop during or after an infection consistent with COVID‑19, continue for more than 12 weeks and are not explained by an alternative diagnosis.
It is believed that Long Covid is caused by immune system alterations secondary to an initial infection. This causes chronic low-grade inflammation with or without increased histamine release, and increased blood clotting.
Individuals with Long Covid may experience clusters of symptoms, often overlapping, fluctuating, and changing over time. The symptoms can range from mild to debilitating and may last for several weeks to months. In addition to the severity of the initial infection, previous comorbidities may affect how severe Long Covid symptoms will be.
As described in an article in the British Medical Journal, the ACE2 receptors, which the virus uses to enter the cells, are in multiple areas of the human body. This includes the lungs, gut, heart, brain, and blood vessels and explains why symptoms can appear in many areas. Fatigue, shortness of breath, and joint pain appear to be the most reported symptoms and at this present time, it is not known if vaccines have any effect on ongoing symptomatic Covid-19 or the prevention of Long Covid.
Benefits of personalisation
- There is one on one interaction between practitioner and patient
- Supports the reduction of comorbidities
- Interventions are tailored to individual biochemistry with the use of testing, nutritional and lifestyle assessment, and careful questioning of previous health history
- Prevents the use of inappropriate supplementation
- Protects the patient from drug nutrient interactions from inappropriate supplementation
- Takes into consideration, physical, mental, and spiritual well-being, social determinants, ethnicity, and religious beliefs
- Can be used safely alongside medical intervention
The main goal to work towards is to encourage immune resilience or immune tolerance. It is important to understand that the goal is not to “boost” the immune system, or suppress it. The ultimate outcome is to achieve immune harmony whereby the immune system behaves and acts according to the environment it is exposed to, as opposed to becoming hyperactive.
As previously mentioned, the Covid-19 pandemic has really been a pandemic of the metabolically challenged population groups. So, it is important to encourage the reduction of risk factors, inflammation, and oxidative stress which are all responsible for causing the inappropriate behaviour of the immune system.
A particular model has been adopted here in the UK by BeNourished, which covers the important holistic elements to address the susceptibility and severity of illness and support immune tolerance through personalised nutrition and lifestyle interventions.
The specific areas of focus through personalised nutrition and lifestyle interventions
- Nutrition and Hydration – Lifestyle Interventions # 1
- Metabolic Flexibility – Lifestyle Interventions # 2
- Microbiome Harmony – Lifestyle Interventions # 3
- Physical Fitness – Lifestyle Interventions # 4
- Mental Wellbeing – Lifestyle Interventions # 5
Lifestyle Interventions
Nutrition and Hydration
It is important that people suffering from Long Haul Covid have access to a multi-disciplinary team depending on the severity of symptoms. Working closely with GP’s exercise specialists, physiotherapists, psychologists, or ear nose, and throat specialists dramatically improve health outcomes.
From a nutritional standpoint, performing a detailed health questionnaire, undertaking dietary analysis and body composition assessment can use useful when tailoring individualized programs.
Appropriate access to testing, ongoing dietary counseling, and supplementation may be needed, and nutrition plans must be designed based on careful consideration of macro and micronutrients. Other considerations include optimizing the intake of polyphenols, phytonutrients, antioxidants, and foods that support the gut microbiome. A special focus should be placed on Vitamin D, Omega-3 Fatty acids, and protein requirements.
To build a healthy nutrition plan, first focus on plenty of non-starchy vegetables, the key here is to include color and diversity to increase antioxidant production and help support gut health. Next build in starchy vegetables, possibly grains, and fruits, to support gut health as well as mitochondrial recovery and energy production. Next, build in protein requirements based on body composition. For instance, if a patient has lost a lot of muscle mass, protein requirements may need to be increased beyond standard guidelines to facilitate the repair and regeneration of lost tissue. Next, include good healthy sources of fats with a focus on the omega 3 fatty acids to support inflammation signaling. These lifestyle interventions provide the building blocks on which further personalization can be adopted depending on the clinical presentation of the client and their symptoms.

Lastly, the impact that the loss of taste and smell not only takes away the joy of eating but can suppress the appetite, therefore having a negative impact on the food choices that are made.
With regard to hydration, there are no real recommendations. 8 glasses of fluid a day tend to be the general guideline, however, all dietary and hydration-related lifestyle interventions need to be made in accordance with individual health requirements, while applying caution to kidney health which can be damaged as a lasting effect of Covid-19 infection.
Metabolic flexibility
What is metabolic flexibility?
Metabolic flexibility means if someone is metabolically flexible, they have a higher chance of achieving homeostatic balance in the presence of a stressor, rather than pushing towards a scenario of chronic low-grade inflammation. Chronic stress is a major source of low-grade inflammation and the way that the body’s metabolic flexibility handles stress is the same irrespective of whether that stress is physiological or psychological.
The particularly impressive diagram above designed by Tom Guilliams, Ph.D., depicts beautifully the 4 major quadrants that need to be supported to achieve metabolic flexibility.
Circadian quadrant
Within the circadian quadrant, poor sleep, shift work, jet lag, and excessive caffeine can exacerbate stress.
Inflammation quadrant
In the inflammation quadrant, environmental toxicity, pre-existing conditions, poor gut health or latent / reactivated pathogens can exacerbate stress.
Glycemic quadrant
In the glycemic quadrant blood sugar irregularities, poor diet, sporadic meal timings, insulin/leptin resistance, emotional eating, and a sedentary lifestyle can exacerbate stress.
Stress quadrant
Then in the perceived stress quadrant, external sources of stress, from challenging relationships, work-related stress, financial worries, burnout, or lack of control, can exacerbate stress.
To promote metabolic flexibility, all these areas will need to be addressed. Some individuals may be more dominant in a specific quadrant, however, each quadrant can be addressed for metabolic flexibility. With dietary and lifestyle interventions, metabolic flexibility can be achieved.
Microbiome Harmony
Wherever there is a mucous membrane there is a unique and diverse set of microbes that interact symbiotically together and provide our first line of defense against foreign invaders. There is a microbiome within the nose, mouth, throat, lungs, stomach, gut, urinary system, and reproductive tract. What has been exciting to discover over the last couple of years, is that the individual microbiomes within these areas seem to communicate with each other, working together to support the immune system and prevent inflammation. This knowledge makes the microbiomes an attractive area to support when looking to improve not only the recovery from Long Covid but also the resistance and resilience to further infection.
The oral, nasal, gut, and lung microbiomes have a particular role to play in respiratory infections and there are several ways that these microbiomes can be supported. It is now well established that pathogenic bacteria in the mouth can cause problems in other areas of the body, therefore improving oral hygiene will favor the production of a good healthy microbiome in the mouth. This can be achieved through regular flossing and brushing, reducing sugar and alcohol intake, keeping up with dental hygienists, or having holistic dental appointments.
Sinus washes and steam inhalation can help remove debris from the sinuses and nasal cavities. There has been some suggestion that antiseptic nasal sprays, povidone-iodine, and hydrogen peroxide sprays may be useful. The caveat to antimicrobial sprays is that they can also displace the beneficial microbes and therefore should not be used on a long-term basis.
There are several ways to support the gut microbiome using foods, such as pre, pro, and post-biotics-rich foods to encourage the growth and proliferation of healthy microbes, supplementation can be used but only under the guidance of a qualified professional, and the simple act of supporting the oral and nasal microbiomes may, in turn, have a beneficial effect on the gut.
Supporting the lung microbiome can be a little trickier as there is not a lot of research in this area, however, steam inhalation and some herbal formulas can support the removal of debris and excess mucous from the lungs. Emerging evidence is suggesting that the lung and the gut microbes operate on a feedback loop, so any imbalances in the gut can affect the microbiome in the lung and vice versa. More research is to come on this and the implications it could have on future respiratory illnesses.
Exercise and movement
There is no denying that exercise has a beneficial impact on physical and mental health. However, exercise fatigue has become a common complaint in many long haulers and even athletes have been affected.
Firstly, rest is the best remedy post covid infection. Even if there have been no symptoms during the initial stages of infection, it may be sensible to rest or at least takedown activity levels to a gentler pace for a few days. It is not yet known whether there are any underlying inflammatory processes occurring in asymptomatic patients.
Those with more severe symptoms may need to rest for longer following the initial infection and ease back gently into formal exercise, starting out with gentle movement and stretching, building up to walking and then previous activities. This is where the help of an exercise specialist and physiotherapist will be beneficial.
Mental wellbeing
It has been suggested that Covid-19 can be more prevalent in patients with mental health conditions, and this could be linked to poorer immune defenses. Recovery from Covid-19 can also lead to an increase in psychiatric disorders, particularly if the patient was exposed to a traumatic experience during the illness. There are many routes to achieving stability, referral to a GP, psychologist, and additional services such as cognitive-behavioral or talking therapy are highly beneficial.
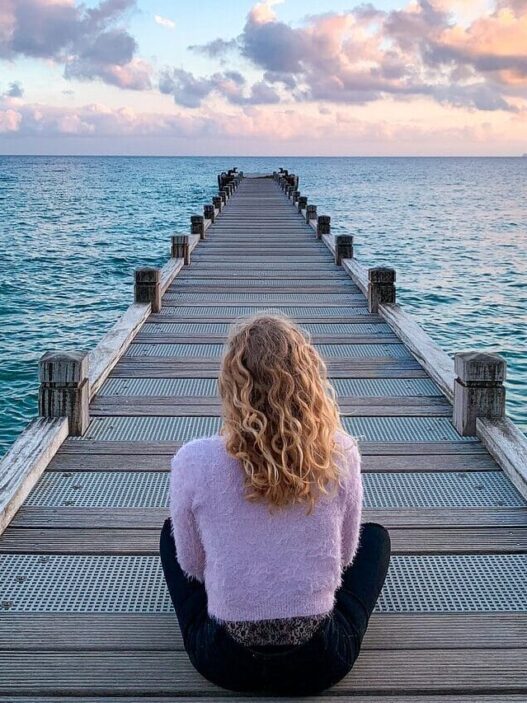
Some holistic approaches that can be considered alongside the above interventions include nurturing connections. A good one to start with is a connection to nature. This can be particularly helpful for those suffering from anxiety and depression. 10 minutes a day of focusing the senses on the sounds smells and the feeling that nature can become very grounding and calming. Being in nature helps to activate the parasympathetic nervous system responsible for balancing out stress responses. Other benefits include breathing in the fresh air and being exposed to the healing rays from the sunshine that produce vitamin D, which is not only beneficial for mental health but also for the immune system.
Faith, worship, and prayer, either individually or as part of a collective, bring about a connection to God or spirituality and can be a powerful tool in supporting mental well-being. Individuals who are not connected to a particular faith will find that meditation, non-religious prayer, positive affirmation, and meditative practices such as yoga or sound emersion are just as effective.
Our close bonds are beneficial for our mental health and wellbeing, nurturing the connections between family members, friends, and even pets makes challenging times easier to navigate.
Finally, a reminder that connection to self is one of the most important connections we can have. All humans tend to turn to external sources to save the day, however connecting with the body which has come equipped with powerful healing abilities and understanding that what goes in, on, and around the body is controllable, places focus on the individual responsibility that is needed to support health and wellbeing.
Conclusion
In summary, these 5 areas of personalized nutrition and lifestyle interventions focussing on nutrition and hydration, metabolic flexibility, microbiome harmony, physical fitness, and mental wellbeing can all determine which risk factors patients present with and the level of inflammation and oxidative stress they experience.
By personalizing interventions and optimizing these key areas through lifestyle interventions, patients will become much more resistant and resilient to illnesses and will likely recover quickly. Ongoing nutrition and lifestyle support are needed to enhance motivation and further improve long-term outcomes.
Sources
Asadi-Pooya AA, Akbari A, Emami A, et al. Risk Factors Associated with Long COVID Syndrome: A Retrospective Study. Iran J Med Sci. 2021;46(6):428-436. doi:10.30476/ijms.2021.92080.2326
Cereda E., Clavé P., et al,. 2021. Recovery Focused Nutritional Therapy across the Continuum of Care: Learning from COVID-19. Nutrients 13(9):3293.
Cleary DW, Clarke SC. The nasopharyngeal microbiome. Emerg Top Life Sci. 2017 Nov 30;1(4):297-312. doi: 10.1042/ETLS20170041. PMID: 33525776.
Crook H, Raza S et al., 2021. Long covid—mechanisms, risk factors, and management BMJ 2021; 374,n1648
Fernández-Lázaro D, Sánchez-Serrano N, Mielgo-Ayuso J, García-Hernández JL, González-Bernal JJ, Seco-Calvo J. Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic? J Clin Med. 2021 Dec 11;10(24):5799. doi: 10.3390/jcm10245799.
Guilliams T., 2015 The Role of Stress and the HPA Axis in Chronic Disease Management . Point institute p382
Hanada, S., Pirzadeh, M., Carver, K. Y., & Deng, J. C. (2018). Respiratory Viral Infection-Induced Microbiome Alterations and Secondary Bacterial Pneumonia. Frontiers in immunology, 9, 2640.
Jimeno-Almazán, et al. (2021). Post-COVID-19 Syndrome and the Potential Benefits of Exercise. International journal of environmental research and public health, 18(10), 5329.
Liu Q,. et al,. (2021) Gut microbiota dynamics in a prospective cohort of patients with post- acute COVID- 19 syndrome BMJ 0:1–9. doi:10.1136/gutjnl-2021-325989
Maki KA, et al. (2021) The Oral and Gut Bacterial Microbiomes: Similarities, Differences, and Connections. Biol Res Nurs. 23(1):7-20
Mitchell, F., (2020) Vitamin D and Covid-19: Do deficient risk a poorer outcome? The lancet. Diabetes & Endicrinology. 8(7):570
https://www.cuh.nhs.uk/news/friendly-gut-bacteria-speeds-long-covid-recovery
NICE., (2022) Covid-19 Rapid guidance: Managing the long-term effects of Covid-19 v1.13 Published 02/01/2022 https://app.magicapp.org/#/guideline/EQpzKn/section/n3vwoL
O’Dwyer, D. N., Dickson, R. P., & Moore, B. B. (2016). The Lung Microbiome, Immunity, and the Pathogenesis of Chronic Lung Disease. Journal of immunology (Baltimore, Md. : 1950), 196(12), 4839–4847. https://doi.org/10.4049/jimmunol.1600279
Taquet, M., Luciano, S., Geddes, J. R., & Harrison, P. J. (2021). Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. The lancet. Psychiatry, 8(2), 130–140. https://doi.org/10.1016/S2215-0366(20)30462-4
Thacher, T.D., 2022. Evaluating the Evidence in Clinical Studies of Vitamin D in COVID-19. Nutrients 2022, Vol. 14, Page 464, 14(3), p.464.

Rachel Jessey holds a Master’s Degree in Personalised Nutrition and Diploma in Nutritional Therapy. She has undertaken extra training in Function Medicine and has a keen interest in the immune system and autoimmune conditions. As well as conducting ongoing research for various companies, Rachel runs a busy eConsult clinic in the UK and has been in clinical practice for over 12 years.