What is Genitourinary Syndrome of Menopause?
The genitourinary syndrome of menopause is a condition that can go on for years, hidden, due to embarrassment and due to the belief that this is a normal part of aging for women. It takes careful, sensitive questioning to encourage a woman to admit that she suffers from these genitourinary symptoms and urogenital atrophy. Also, to explain to her why it is happening and inform her that vaginal estrogen treatment is safe for almost every woman, is long-term, and is effective.
Genitourinary syndrome of menopause is experienced by 60% of postmenopausal women who do not use hormone replacement therapy (HRT), and 25% of women who do use systemic hormone HRT. As other symptoms of menopause can settle, the genitourinary symptoms do not unless treated appropriately.
From what genitourinary symptoms do women suffer?
The genitourinary symptoms that women suffer in the genitourinary syndrome of menopause include –
- Vaginal discharge
- Vulval/vaginal dryness
- Pain during sexual intercourse
- Decreased arousal, orgasm
- Vaginal bleeding
- Urinary urgency
- Urinary incontinence
- Urine infections
- Tissue shrinkage
What do women say when asked if they have genitourinary problems involving discomfort around the vagina or vulva?
In the genitourinary syndrome of menopause, women usually complain about the discomfort around the vagina or vulva as mentioned below –
- ‘It’s so itchy, I can’t stop scratching’
- ‘It feels so dry’
- ‘I cannot wear underwear it is so uncomfortable’
- ‘It’s so sore’
- ‘It feels prickly’
- ‘It feels like I have cut down there’
- ‘I bleed after sex’
- ‘Sex is so uncomfortable, now’
- ‘I need to pass urine far more often’
- ‘I’m getting urine infections’
- ‘It feels like razor blades’
- ‘It stings to pass urine’
- ‘I keep getting candida infections’
- ‘It’s just agony having my smear test’
Many women feel that they only become dry during sex, which can be painful, while others feel dry, sore, prickly, and itchy all the time. They may even have pain in the vagina and bleed after sex. These genitourinary problems are associated with sexual dysfunction and arousal disorder.
The lower urinary tract is also affected by the genitourinary syndrome of menopause, and a woman can be affected by recurrent urinary tract infections, the urge to pass urine, frequency of passing urine, and dysuria, which means it is painful for her to pass urine.
These genitourinary symptoms are not usually significant until around 10 years after menopause but can present in 3-5 years as estrogen levels start to fall. While vaginal symptoms of urogenital atrophy become more common with age, they can occur at any stage of perimenopause and menopause.
Why does the genitourinary syndrome of menopause happen?
Estrogen is needed to keep tissues well-lubricated, healthy, and supple. Loss of estrogen in perimenopause and menopause results in the tissues becoming delicate and dry.
The usual elasticity of the vagina and vulva can be lost, which can mean sex is painful. The vagina can become shorter and lose its usual folds, especially if a woman stops having sex. All these genitourinary changes are called urogenital atrophy.
Estrogen also stimulates the presence of good bacteria, lactobacillus, in the Vaginome of the vagina, to protect her against vaginal infections.
What might be seen on examination in Genitourinary Syndrome of Menopause?
The vulva appears paler in the genitourinary syndrome of menopause.
Further, the labia are thinner and smaller.
The clitoral hood is less obvious.
A urethral mucosal prolapse can occur which many women notice as a red swelling.
The vulval skin looks thin and dry, with tiny blood vessels under it resulting in patchy redness.
Stretching the vulva may cause splitting at the skin at the bottom of the vagina or around the anus.
How does the vagina change after menopause?
The genitourinary syndrome of menopause also include vaginal changes as mentioned below –
The vagina before menopause:
The lining is moist and thick.
There is good blood flow to the vaginal tissue.
The vaginal walls are flexible.
The vagina after menopause:
The vagina becomes dry and thin.
There is less blood flow to the vaginal tissue.
Vaginal flexibility reduces.
What do women say happens to their relationships if they suffer from Genitourinary Syndrome of Menopause?
Led to loss of intimacy in 85%
Detracted from the enjoyment of sex in 59%
Interfered with the relationship in 47%
Negatively affected sleep in 29%
Adversely affected general enjoyment of life in 2.7%
What advice and treatment can be offered for Genitourinary Syndrome of Menopause?
Non-soap cleanser
A non-soap cleanser can be used or advised to gently wash with warm water alone, no more than twice daily if you have the genitourinary syndrome of menopause.
Do not use harsh products
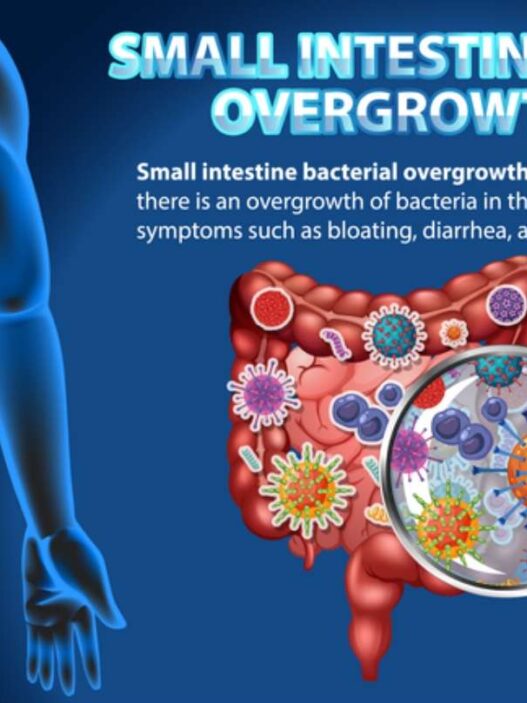
It is important not to douche or use harsh products as these affect the vaginal pH. The premenopausal vaginal pH is around 4.5 and the post-menopausal vaginal pH naturally rises. This is due to the falling estrogen levels, which affects the microbiome in the vagina, called the vaginome, the main effect is a reduction in lactobacillus.
Lactobacillus has a very important role in protecting the vagina from bacterial, viral, and candida infections and keeps the vagina healthy, by making it more acidic. It achieves a lower vaginal pH by producing lactic acid when it ferments glycogen in the body. If levels of lactobacillus are low, as they can be after menopause, it can be easier to suffer from candida, BV and other infections.
If candida is allowed to multiply this is called vaginosis, it can produce an unpleasant fishy odour due to the production of a substance called trimethylamine.
Emollient cream
An emollient cream or petroleum gel can be used for genitourinary symptoms involving a dry and itchy vulva.
Emollients that can be considered are Cetreban, Dermol, Diprobase, Doublebase, Epaderm, Hydromol, Zeroderm, and Vaseline. Aqueous cream is best avoided as it can irritate.
Lubricant
A lubricant can be used for sexual intercourse, this does not contain estrogen, and if it stings she can use another brand or use petroleum gel.
Oil-based lubricants can be more effective for genitourinary problems, though they can make condoms less effective, so if she uses condoms she should use a water-based lubricant. The key thing is finding one she likes.
Examples are YES OB or YES WB. It’s important to look for a recommended brand. She should avoid lubricants with added extras (like a tingle, or heat) as they can cause more irritation. Shop-bought products can irritate, so care is needed. A good website is Jo Divine to look for products.
Vaginal Moisturizers
A trial of vaginal moisturizers, using a reputable brand is also really helpful for genitourinary symptoms. They are helpful throughout the day and can be applied as needed. YES VM and Sutil Luxe and Rich are good products.
Avoiding products that contain glycerine or glycerol is best as these may exacerbate thrush. Ovestin local estrogen cream contains glycerin so care may be needed with this.
Women can review their medication with a doctor. Anticholinergic medication, antihistamine, a decongestant, or antidepressant medication may be contributing to dryness, if taking these, women can consider stopping them.
Short-term topical steroids may be necessary for dermatitis caused by irritants such as urine, panty liner, or tight clothing.
Local vaginal estrogen can be used.
Why is vaginal estrogen used, instead of applying it to the vulva?
There are more estrogen receptors in the vagina than in the vulva so it makes sense to do this.
Vaginal Estrogen
Vaginal estrogen use will help by increasing the vaginal lactobacillus, and subsequently lowering the vaginal pH again, which will be having a beneficial effect on the vaginome. It will improve the quality of the skin on the vulva and vagina and help with improving prolapse and bladder/ genitourinary symptoms. Urinary contact with the vulva and pads causes the most challenging symptoms topical steroids may also be needed to help if things are severe.
Local or topical or vaginal estrogens can be prescribed in the form of Estradiol (E2) or Estriol (E3) safely in almost every woman, even if they take systemic HRT. These can be given as a cream, a gel, a pessary or vaginal ring, inserted into the vagina with a finger, or a small applicator. A loading dose is given and this is followed by a maintenance dose for most preparations.
It is best if treatment is started early, when genitourinary symptoms are mild, as it is much easier to keep tissues healthy than it is to try to reverse the changes in the skin that have been there for years, but it is never too late to start. It usually takes three to four months for improvement to be felt. Vaginal estrogen is used long-term to prevent genitourinary problems with an annual review. There is no evidence one vaginal estrogen is better than another.
Women often ask about the safety of using estrogen. It’s reassuring to know that when they put estrogen directly into the vagina, their body only absorbs a tiny amount. So, they can use it without the risk of breast cancer, blood clots, stroke, or heart disease. They do not need to use progesterone treatment to provide endometrial protection if they only use local estrogen.
There are different options available for vaginal estrogens, as shown in the table below. The dosing varies for all of them and will be confirmed on their prescription.
If the symptoms do not improve using one product, then two products can be combined together, one estriol and one estradiol, as this may help. Systemic HRT may need to be added, too.
Vaginal estrogen products available
- Vagifem TM or Vagirux -Estradiol 100mcg vaginal tablet. These are tiny pessaries with an applicator that can be reused and washed.
- Imvaggis TM – Estriol 30mcg pessary. This is a slightly bigger pessary. There is no applicator, it is inserted using the woman’s finger to push it into the vagina. It melts and some women find it moisturizing.
- Ovestin cream TM – Estriol 0.1% cream. This comes with a washable applicator, but you could measure out the applicator dose and use your finger instead.
- Estriol 0.01% cream. This is a cream, and it comes with a washable applicator, but you could measure out the applicator dose and use your finger instead.
- Blissel TM – Estriol 50mcg. This is the lowest dose of vaginal estrogen; it comes in a tube and is drawn up into an applicator.
- Estring TM – Estradiol 7.5mcg/24h. This is a small flexible plastic ring that is fitted into the vagina, by the doctor or by the woman, and it releases estrogen slowly daily for three months. It needs to be changed every 3 months, but it can be taken out and washed during this time if necessary. She can continue to have sex with this fit.
There are two other medications used to treat genitourinary vaginal symptoms related to urogenital atrophy of menopause. They are usually prescribed by specialists and to be taken only if your doctor recommends.
Medicines for Urogenital Atrophy
- Prasterone (Intrarosa TM) is a 6.5mg pessary containing DHEA delivered vaginally daily. It’s identical to a hormone called dehydroepiandrosterone (DHEA) in the adrenal gland. The adrenal glands (80%) and ovaries (20%) secrete DHEA. It is converted into estrogens and androgens by enzymes within the epithelial cells of the vagina, but not the endometrium. It causes the maturation of the parabasal cells into superficial cells, with an associated increase in mucosal thickness and secretions. It increases collagen density in the lamina propria. This has been shown to be effective in treating menopausal vaginal and vulval atrophy (thinning) that is moderate to severe.
- Ospemifene is an oral tablet administered at a dose of 60mg once daily. It is a selective estrogen receptor modulator that has an estrogen-like receptor effect on the vagina, increasing cellular maturation of the vaginal epithelium and lowering the vagina pH, and improving the vaginal maturation index (VMI). It reduces symptoms including vaginal dryness and pain during sexual intercourse. There is an antagonist effect on the endometrium and breast tissue. Hot flushes are most frequently reported as a side effect of this medication. NICE guidance recommends its use for women who are not candidates for local estrogen therapy. 52-week extended studies showed long-term benefits from long-term use.
Vaginal dryness can make women more prone to vaginal candida infections and discharge can decrease or increase as the balance of bacteria that are naturally found in the vagina changes.
Women may also be more prone to bacterial vaginosis, where there is an imbalance of the normal bacteria that usually live happily in the vagina. Excessive vaginal discharge can sometimes cause further irritation.
Low-dose vaginal estrogen can be used safely and continued for as long as required. Genitourinary symptoms of vaginal atrophy often come back when the treatment is stopped, adverse effects are very rare, and any unscheduled bleeding should be reported to their doctor.
Vaginal laser therapy
Vaginal laser therapy is a technique that may help the symptoms of vaginal atrophy. Laser energy is used to treat vaginal tissue and increase collagen production. Results from small studies have shown that this treatment can be effective, but it is not yet widely available.
Chronic vulval irritation is another genitourinary symptom that is extremely debilitating and has a significant effect on mood, well-being, and relationships. A doctor should examine the vulva and assess for inflammatory skin disorders or malignancy.
Final Words
It is so important that every woman is counseled about the genitourinary syndrome of menopause early so that they can start treatment for the genitourinary syndrome of menopause before symptoms cause a problem for her and her relationship.

Dr. Carys Sonnenberg is an NHS GP with a special interest in Women’s Health and Menopause. She runs an NHS women’s health clinic at her practice. She is a British Menopause Society trained doctor and is completing the advanced menopause training to become a BMS Menopause Specialist. She is the founder of Rowena Health, which she runs, and enables her to offer private appointments to women for holistic menopause care, all over the UK. She is passionate about education and sits on the Education Committee for the Primary Care Women’s Health Forum. In her free time she loves walking her dog and spending time outdoors with family and friends.