Menopause, the second flowering in life, is a time to flourish and bloom for EVERY woman. If we all enlighten ourselves, doctors, wives, husbands, daughters and sons about Menopause and hormone replacement therapy (HRT), together we can help to diagnose early and to support holistically all those women whom we love. Check out the advice of a menopause doctor on symptoms of menopause and how you can manage using HRT.
47 million women each year become menopausal, 25% of them have severe symptoms and 77% of those do not realize their symptoms are due to menopause.
I’m Dr Carys Sonnenberg, the menopause doctor. I have a love of learning, and this has been part of the reason being a doctor suits me so well and has led to my passion for menopause. I became perimenopausal when I was 45, after three months of drenching night sweats, insomnia, irritability and a brain fog meaning I could no longer concentrate for more than a few minutes to enjoy reading or learning from medical articles, the penny dropped for me. I missed my cognitive function the most. I visited my GP who wondered if I had lymphoma.
As I had lost weight, he wanted to investigate with a blood test, but I felt I knew my body and after some discussion, I persuaded him to prescribe hormone replacement therapy, HRT, and quickly my night sweats stopped. Gradually, I felt better about myself over the months that followed. I did need to increase my dose of oestrogen after consulting a menopause doctor as my symptoms fluctuated over the first couple of years. The whole experience changed my life. I began to speak about menopause and hormone replacement therapy, HRT to everyone I knew, to gain from their experiences. I spoke about it incessantly at work, I got everyone talking about it, which was great!
I injured my knee skiing in February, as I am not one to sit around and do nothing. I started posting information for education about menopause on my new Instagram site. Four days ago, I had an operation to repair the ruptured ACL in my injured knee, so I wrote this article while resting and recuperating. A perfect way to fill my time and to show my support for the hot topic, that is, Menopause.
To enlighten is to give someone greater knowledge and understanding about a subject. It seemed the perfect word to explain my aims for education and menopause.
Empathy, as a menopause doctor and a woman with a personal journey through menopause, makes some of my patient’s phrases stick in my mind:
‘I wish I’d known I was perimenopausal last year before my husband left me and my family as I was just so angry all of the time.’
‘I wish I’d known the way I’ve been feeling that caused me to resign from a job I loved as I couldn’t cope anymore, was the menopause.’
‘I wish I’d known I could have had HRT even though my Mum had spontaneous breast cancer, as my risk is not raised.’
‘I’m just so grateful you have listened, and that we have a treatment plan in consultation with a menopause doctor that suits me with HRT and a future plan to check I’m ok, I understand it now. My children say that they think I am like Mummy again, I’m so grateful.’
‘Thank you, I thought I’d have to fight to get this treatment, my friend’s GP won’t give it to her’.
Each of these comments I have listened to, through tears of anguish, regret or relief. Empathy just is not enough. Early enlightenment, education, understanding and empowerment, are enough.
For this reason, I am calling all Menopause Doctors to THINK MENOPAUSE for every Female in their Forties. We must be vigilant, we must take time, but sadly, on the NHS is not something we have the luxury of, with only 10 minutes of consultation time per patient, but we must.
There are a plethora of menopause doctors offering private menopause consultations. Not every woman has the money to pay for this, nor should they have to, but EVERY woman WILL go through this. Education of EVERY WOMAN is the key as well as more education for EVERY MENOPAUSE DOCTOR.
I didn’t have specific menopause education. I have chosen to do menopause courses to become a menopause doctor. I plan to attend the British Menopause Society (BMS) 2-day conference in June; to complete the BMS menopause course and CBT for hot flushes BMS course in September. I am a member of the BMS and an Associate of the Newson Health Menopause Society.
Not every GP will have the same passion for this topic to be a menopause doctor, they will embrace other interests. As GPs, every 10 minutes a different challenge walks through our door, during morning surgery, and it is upon these challenges we thrive.
As we train, we won’t get it right all of the time, we support, we teach, we learn, and we are passionate about that. That is what makes us choose medicine. I realize that there is a huge gap in our training with the lack of menopause training. We must address this, we must THINK MENOPAUSE, it needs to become the heart of every female consultation for women in their 40s.
PERIMENOPAUSE?
The time before menopause, when you have symptoms but still have periods.
MENOPAUSE?
You have not had a period for over a year, now the average age is 51. Your ovaries no longer produce eggs and as a result the levels of hormones, oestrogen, progesterone and testosterone fall. Oestrogen receptors are on every cell in our bodies, so the symptoms can be variable. Menopause means living with a long-term chronic hormone deficiency.
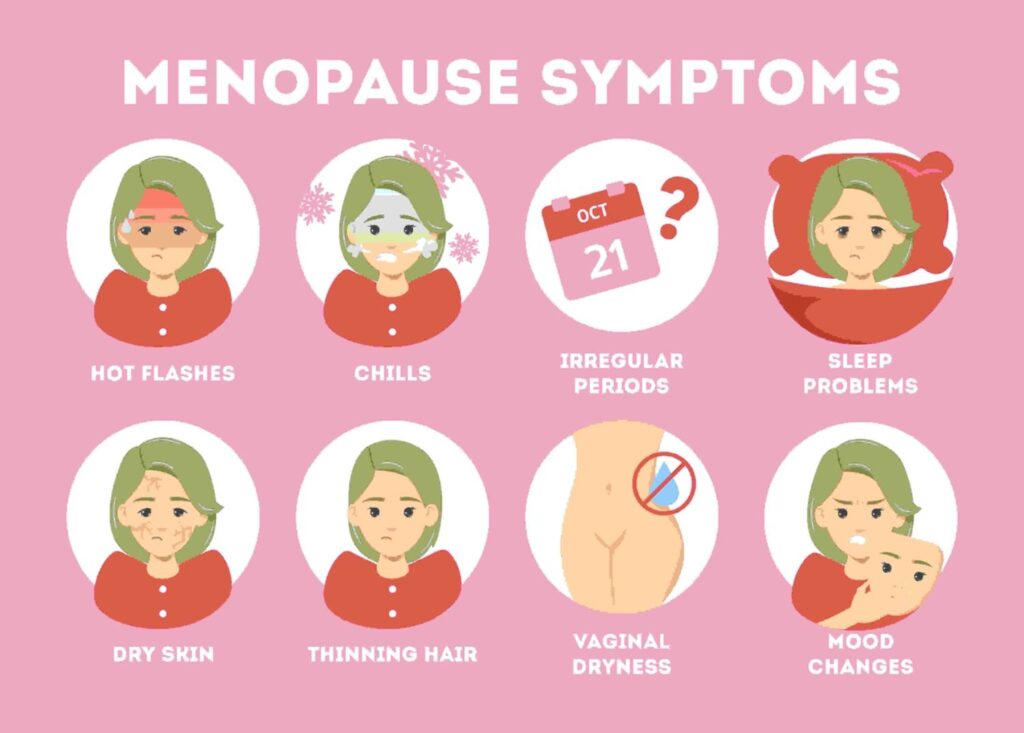
SYMPTOMS OF MENOPAUSE AND PERIMENOPAUSE
GENERAL PROBLEMS
- Daytime sweats and flushes?
- Nighttime sweats and flushes?
- Unable to sleep?
- Headaches, pressure, tightness in the head or worsening migraines?
- Tiredness/fatigue?
- Breathing difficulties?
- Loss of energy?
- General aches and pains in joints and muscles, as oestrogen is an anti-inflammatory?
- Brittle nails?
- General itchiness or a feeling of something crawling on you?
- Thinning hair and dry skin?
- Burning mouth?
- Dry eyes?
- Worsening Irritable Bowel Syndrome, bloating?
- Increase in allergy symptoms or hay fever?
- Noise sensitivity or tinnitus?
- Loss of feeling in hands or feet or parts of the body feeling numb?
- Feeling dizzy or faint?
- Breast soreness?
- Weight gain?
- Body odour?
EMOTIONAL PROBLEMS
- Tearfulness?
- Low mood and feeling unhappy?
- Loss of interest in things?
- Feeling of unworthiness?
- Irritability?
- Anger?
- Bitterness?
- Panic attacks +/- palpitations?
- Aggression?
- Feeling tense or nervous, a common problem is a lack of confidence driving on the motorway.
- The feeling of the heart beating quickly or strongly?
The madness of menopause in history and literature can be seen with Shakespeare’s witches in Macbeth and Bertha Mason in Jane Eyre.
Mindfulness and meditation can help rest your brain from the cognitive changes experienced at this time.
BLADDER PROBLEMS
- Daytime frequency?
- Urgency? (Having to dash to the loo).
- Urge incontinence? (Leakage if you don’t get there in time).
- Stress incontinence? (Leakage as you jump, run, laugh or cough).
- Nighttime frequency?
- Bedwetting?
- Recurrent Urine infections or cystitis?
Please avoid caffeine and fizzy drinks, and drink 8 glasses of water a day. Lots of women drink less, as they don’t want to leak. This makes it worse as you may develop a urine infection or become dehydrated. Don’t forget to do your pelvic floor exercises.
SEXUAL PROBLEMS
- Vaginal soreness?
- Dryness and itching, it might be very sore to have your smear done. Please talk with your older relatives, most never complain about this, they are too embarrassed, even if it’s very sore. It is never too late to start local oestrogen which will really help. The local oestrogen keeps the vagina healthy; it is a natural lubricant and stimulates the vagina to encourage good bacteria. It is completely safe for almost EVERY woman.
- Soreness to pain during sexual intercourse. Please use a vaginal moisturizer twice a week and a lubricant when you have sex. It will help.
- Loss of sex drive? Have you spoken to your GP about Testosterone treatment?
- Difficulty achieving an orgasm?
Vaginal tissues have two types of oestrogen receptors, Estriol and Estradiol. There are creams, gels, pessaries, and a small flexible plastic ring containing either type of oestrogen which can safely be prescribed by menopause doctors to help vaginal and bladder symptoms and can be used FOREVER with NO RISK in most women.
Some women need both types of oestrogen and also a vaginal moisturizer to help with soreness and itch down there. If you are finding your treatment hard to apply, because of dexterity or messiness then please ask us for a different type, that might suit you better. Don’t forget to use a lubricant when you have sex, it will help, and use a water-based one if you use a condom. HRT is NOT a contraceptive.
BRAIN CHANGES
- Loss of memory? Oestrogen has a neuroprotective effect and promotes neuronal and oligodendrocyte survival and testosterone reduces amyloid deposition in the brain.
- Loss of concentration?
- Inability to cope?
- Brain fog?
PERIOD CHANGES
- Periods are lighter or heavier?
- Irregular periods and irregular spotting in between?
- A new bleed over a year after your periods have stopped? Please see a Doctor about this.
ANDROGENIC SYMPTOMS
- Central obesity?
- Hirsutism (excess hair growth)?
- Thinning hair?
- Acne?
Our oestrogen and testosterone levels drop as our ovaries produce less, but 50% of our testosterone is produced by our adrenal glands, so the balance of these hormones changes causing these symptoms.
Please speak with your GP or menopause doctor about your symptoms to discuss an individual treatment plan.
We are all individuals, and we all have different health and treatment beliefs. You can explore these by looking at HRT and alternatives to HRT with your GP/ menopause doctor. We can signpost you to a plethora of apps and websites now for you to research yourself and decide what route you will take, depending on your health and risk factors.
We have many things to cover in a consultation to help us decide on the best treatment for you, as an individual. We should ask you about your symptoms, so it helps to write these down. We should explore your health concerns and ask about your lifestyle, diet (calcium intake), exercise, smoking, and alcohol intake. Your medical history, for example, blood clots, migraines, breast cancer. Your family history for example of breast cancer. Your mental health. Your risk factors for cardiovascular disease or osteoporosis.
What supplements do you take? Do you require contraception? How have you managed contraception in the past? Might you be progesterone sensitive? Have you taken HRT before and so much more? Menopause doctors are looking at risks and benefits for you as an individual. We are also looking to educate you about your health and lifestyle. This may take a few consultations, it cannot all be covered in 10 minutes.
For menopause, briefly, there are only two herbal treatments for which good evidence exists for vasomotor symptoms: Black Cohosh and St John’s Wort, but these really can interact with other medications so please do tell us if you want to consider these. I have not discussed alternatives to HRT here but there certainly are some, if HRT is not a choice for you.
RISKS TO YOUR HEALTH WITH THE MENOPAUSE
- Bone loss
- Osteoporosis
- Osteoarthritis
- Sarcopenia
- Rheumatoid Arthritis
- Heart disease
- Type 2 Diabetes
- Obesity
- Cognitive decline and early dementia
- Clinical depression
WHAT IS HORMONE REPLACEMENT THERAPY – HRT?
Hormone replacement therapy (HRT) is formed of oestrogen, progesterone or progestogen, and sometimes testosterone. HRT isn’t actually a replacement though, it is a treatment to top up your hormones to the female level at which they previously were before your ovarian function declined. There is no maximum length of time for which you can take HRT. Taking hormone replacement therapy, HRT, in consultation with your menopause doctor, does not delay your menopause.
OESTROGEN
This can be taken in a gel, a patch a spray that rubs onto the skin and is absorbed into the bloodstream, or an oral tablet. Transdermal oestrogen is absorbed through the skin and is body identical, it is 17 beta oestradiol and derived from yam plants. Taking transdermal oestrogen, after consulting your menopause doctor, does NOT increase your risk of blood clots, as the oral oestrogen tablet can.
Please remember that transdermal HRT under the age of 51 has no risk of blood clots and no risk of breast cancer. It is absorbed differently in every woman, some need much higher doses than others to achieve symptom relief, don’t worry.
Oestrogen can also be taken as a tablet but does have a small risk of a blood clot if taken this way.
PROGESTERONE OR PROGESTOGEN
This is essential if you have a uterus and you take oestrogen, in order to protect the endometrium from thickening.
Utrogestan, is a microgenised progesterone, a body-identical progesterone, which has the same molecular structure as that of our own progesterone and is derived from the Yam plant. It is wonderfully sedative and taken at night on an empty stomach. It can improve cardiovascular risk and lipids, it does not affect BP, has no risk of blood clot, and for the first 5 years has no increased risk of breast cancer. You may consider this after consulting your menopause doctor.
An alternative might be a synthetic progestogen like that coating your Mirena IUS (intrauterine system), which is recommended for 5 years by the FSRH for endometrial protection.
TESTOSTERONE
It is the most abundant biologically active hormone in women. Testosterone receptors are everywhere, as are oestrogen receptors. They are in our breasts, heart, blood vessels, gastrointestinal tract, lungs, brain, spinal cord, peripheral nerves, bladder etc.
Women produce three times as much testosterone as oestrogen before menopause. Falling levels lead to lack of energy, brain fog and low sex drive. It can help with cognitive function and quality of sleep, as well as muscle mass and bone strength. Many women find these things improve if they take Testosterone as part of HRT.
UK guidelines NICE and BMS only recommend Testosterone if you have severely low libido. It is not licensed in the UK for women, but GPs/ menopause doctor is increasingly aware that there are widespread benefits to replacing this hormone. We can prescribe this, if we take full responsibility for your prescription, as we have to do with all unlicensed medications.
You do not usually need to have a blood test before starting treatment and the dose can be monitored by doing blood tests at 3-6 monthly intervals to ensure your FAI (free androgen index which is calculated using SHBG and total testosterone) remains in the female range.
It is available as:
Androfeme cream – 1% testosterone cream in 50ml tubes, this is only available privately. It is made for women and is imported from Australia, under a special license from the MHRA, and is a regulated preparation, but not for women with almond allergy. The starting dose is 0.5mls a day so each tube should last for 100 days.
Testogel and Testim are 1% testosterone gel’s in 5g sachets and each tube should last you 7-10 days, these are available on the NHS.
THE HEALTH BENEFITS OF HORMONE REPLACEMENT THERAPY, HRT

Reduction in:
- Cardiovascular Disease is the greatest benefit. The earlier a woman starts her HRT, within 10 years of their menopause and below the age of 60. HRT can lower cholesterol.
- Osteoporosis
- Osteoarthritis
- Type 2 Diabetes
- Obesity
- Dementia
THE HEALTH RISKS OF TAKING HORMONE REPLACEMENT THERAPY, HRT
These will be discussed with your GP/ menopause doctor for you as an individual.
Risk of a blood clot:
Oral oestrogen (NOT transdermal oestrogen like gels, sprays and patches) have an increased risk of a blood clot because oral oestrogen leads to activation of coagulation factors. It can also lower libido by increasing SHBG (sex hormone-binding globulin) which binds testosterone and it can increase total blood glucose. I do not offer this treatment unless there is no other option.
Risk of breast cancer:
Hormone replacement therapy, HRT gives a very small increase in the risk of breast cancer but being overweight gives a much much higher risk. Exercise can provide protection when looking at risk. Our lifestyle is so important.
Every woman in the UK has a chance of one in eight of developing breast cancer, this is our background risk if we take no medication. We can increase that risk by drinking alcohol, smoking, being overweight, having a family history of breast cancer, taking combined HRT and taking the combined contraceptive pill.
We can reduce that risk by doing 2.5 hours of moderate exercise per week. Our lifestyle choices matter. As a GP and menopause doctor, we ask these questions of you during your consultation because we know that we can educate you, in order to help you reduce your risk.
REALLY IMPORTANTLY we know that under the age of 51, hormone replacement therapy or HRT does NOT increase the risk of breast cancer, no matter how long you take it. If you start it at age 25 for premature ovarian insufficiency and take it until the age of 51 there is NO increased risk, as you are simply using hormone replacement therapy to top up your female hormones to the level at which they should be.
After a hysterectomy, if women use oestrogen-only HRT then they DO NOT have an increased risk of breast cancer, some studies show the risk is actually reduced.
Using combined HRT (Oestrogen AND progesterone) may be associated with a very small risk of breast cancer, but this is similar to the risk you give yourself if you are overweight or drink a glass of wine every day. The media have misinterpreted the information from studies done in the past which led to many women and doctors being scared of HRT. This has led to a reduction in women taking it and having the huge health benefits associated with it, which is very sad.
The risk of breast cancer from hormone replacement therapy, HRT actually comes from progesterone, not oestrogen. The type of progesterone matters, and we know that using body-identical microgenised progesterone does NOT cause an increase in the risk of breast cancer for the first five years of taking. After five years, the risk is very low. It is also very low for women using older types of progesterone in their HRT.
Body Identical, not Bioidentical hormones?
Body identical hormone replacement therapy, HRT, is the safest and most regulated type of HRT. Many private clinics are using Bioidentical hormones, but these are not subject to quality controls and are not recommended by the British Menopause Society.
What happens then? I’m on HRT and I should be fine.
No, that is not the case. You need regular follow-ups with your GP/ menopause doctor. You may need a blood test to check your hormone levels, your dose may need to be adjusted as your hormones fluctuate. We will want to give your HRT hormones time to work, but if they are not suiting you then we can adjust either the dose or the way we administer the oestrogen or progesterone. You may experience bleeding or side effects like nausea, breast soreness or leg cramps. These often settle down after a few weeks. Please talk with your GP if you are experiencing unexpected bleeding on hormone replacement therapy.
Hormone replacement therapy treats a moving target of fluctuating hormones. Please don’t worry if you need to adjust the dose. There is not a smooth linear decline in oestrogen during perimenopause, but a rapidly fluctuating declining one, so please don’t worry if things take time to settle. It may be a bumpy ride but we will help you to manage it.
Please be confident to call your GP/ menopause doctor to review things, I have patients apologizing profusely for bothering me. You are not bothering me, please never feel that way. It is my job to help you and together we will work to find the best treatment for you, give you the confidence to understand how to manage your treatment, explain why you might have side effects and explain the options for managing them.
Please remember to continue to have regular smears and mammograms. Please remember that HRT is NOT a contraceptive unless you are using a MIRENA IUS, which must be changed every 5 years as part of HRT.
Please help yourself by exercising regularly both to increase your heart rate and to build strength; by eating a healthy balanced Mediterranean diet rich in calcium; by limiting alcohol and stopping smoking; by taking Vitamin D supplements, this is pretty much the only supplement you need to take if you eat a good diet; by spending time enjoying relaxing, hobbies, family and friends.
Change is needed. Medical education should include compulsory menopause training. School education should also include this, it could easily be added to sex education. Girls and boys should be educated about the whole of their fertile lives, not just puberty. In addition, many women become perimenopausal at a time when their children are teenagers, so helping both Mum and teen understand the hormonal challenges they face might help life at home.
Can we consider menopause cafes, hubs with supportive holistic care for menopause, mental health, advice on HRT, and advice on exercise and diet?
GP/ menopause doctor consultations need to be longer, to cover this huge condition.
Luckily, change is here, we are all talking about this, there are many good websites to visit that offer evidence-based information and apps to track symptoms. Employees are now sitting up, realizing the struggles women face to continue working at this time. Things can be put in place to help them. The future is certainly brighter.
The more enlightened we are, the better the outcome for women, for families, for employers, for us all. Shakespeare’s witches need be no more.

Dr. Carys Sonnenberg is an NHS GP with a special interest in Women’s Health and Menopause. She runs an NHS women’s health clinic at her practice. She is a British Menopause Society trained doctor and is completing the advanced menopause training to become a BMS Menopause Specialist. She is the founder of Rowena Health, which she runs, and enables her to offer private appointments to women for holistic menopause care, all over the UK. She is passionate about education and sits on the Education Committee for the Primary Care Women’s Health Forum. In her free time she loves walking her dog and spending time outdoors with family and friends.