SIBO - the real cause of your bloating and how to get rid of it?
SIBO stands for Small Intestinal Bacterial Overgrowth and is one of the most common digestive problems that I see in my practice. I have also experienced SIBO myself following a food poisoning episode so have quite literally had a dose of my own medicine! Check out below why it is important to know about SIBO, what causes SIBO, symptoms of SIBO vs IBS, hydrogen vs methane SIBO symptoms, hydrogen sulfide SIBO, how to eliminate SIBO using antimicrobials, and how to treat SIBO naturally using berberine, oil of oregano, neem, garlic, etc. using biofilm disruptors and SIBO diet considerations and how to prevent relapse.
What is SIBO?
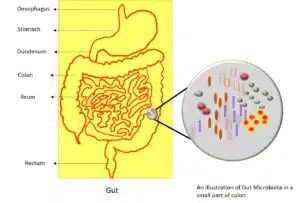
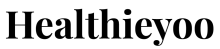
SIBO is Small Intestinal Bacterial Overgrowth and is commonly defined as the presence of excessive bacteria in the small intestine (1). The small intestine facilitates digestion and absorption whereas the large intestine houses our gut bacteria, needed for fermentation of dietary fibre. SIBO is thought to occur when these naturally occurring, non-pathogenic bacteria, normally found in the large intestine, migrate up to the small intestine.
SIBO comes in different forms and may be hydrogen, methane, or hydrogen sulfide dominant. Methane-dominant SIBO is increasingly becoming known as IMO (Intestinal Methanogen Overgrowth). The difference between hydrogen vs methane SIBO and hydrogen sulfide SIBO symptoms is explained. below
Why is it important to know about SIBO?
Symptoms of SIBO often go undiagnosed as they overlap with many other conditions such as Chronic Fatigue Syndrome and fibromyalgia and produce symptoms not always associated with the gut (e.g. brain fog, anxiety, fatigue) (1). Small Intestinal Bacterial Overgrowth or SIBO is a complex gut condition but is treatable.
What causes Small Intestinal Bacterial Overgrowth or SIBO?
SIBO is not a diagnosis in itself but a consequence of underlying dysfunctions or conditions resulting in bacterial overgrowth.
Poor Digestion
Low production of bile, pancreatic (digestive) enzymes, and hydrochloric (stomach) acid. Bile, digestive enzymes, and stomach acid facilitate the digestion and absorption of food and, much like detergent, help to prevent bacterial overgrowth. Some infections such as Helicobacter pylori reduce stomach acid production.
Poor gut motility
Dysfunction of one of the three main components of motility, the MMC (Migrating Motor Complex), the vagus nerve, and the ICC (Interstitial cells of Cajal). MMC, otherwise known as the “housekeeping wave” is responsible for moving food and cellular debris from the stomach and/or small intestine to the large intestine. It is active in between meals when fasting and at night. The vagus nerve runs from the brain to the gut and stimulates tissues needed for digestion and absorption. When we constantly snack, or the nerves or the cells in our gut are damaged as a result of an acute bacterial infection (e.g., Shigella, E. coli, campylobacter jejuni, salmonella) the MMC does not work properly. Undigested food is fermented by bacteria in the small intestine, causing unpleasant symptoms such as bloating. Hypothyroidism, autoimmune disease, TBI (Traumatic Brain Injury), Lyme Disease, Diabetes, Ehlers’s Danlos Syndrome, Parkinson’s Disease, and scleroderma may also result in poor motility.
Poor digestive flow
ICV (ileocecal valve) dysfunction and anatomical or structural obstructions. The ICV, located between the small and large intestine, can stay open too long, allowing bacteria to flow back up into the small intestine. Anatomical obstructions and adhesions can, like a blocked drain, cause a backflow of bacteria from the large intestine to the small intestine. People with obstructions may have had abdominal surgery, have cancer, SBS (Short Bowel Syndrome), PID (Pelvic Inflammatory Disease), diverticulitis, endometriosis, or IBD (inflammatory Bowel Disease).
Medications
PPIs (Proton Pump Inhibitors) e.g., omeprazole prescribed for acid reflux, reduce hydrochloric acid production. Antibiotics and opioid medication disrupt gut bacteria.
Poor oral health
Gum disease or oral infection can result in an imbalance of bacteria, or dysbiosis, in the mouth which can lead to an imbalance of bacteria in the gut.
Environmental toxins
Chemicals, heavy metals, and mycotoxins (mould toxins) can affect the integrity of the gut and result in gut dysbiosis.
Suppressed immunity
SIgA (Secretory IgA), an important part of our immune system, is produced in the gut and prevents bacterial proliferation. Gut dysbiosis lowers SIgA production.
Chronic stress and emotional trauma
Chronic stress lowers stomach acidity, slows down the movement of food through the gut, damages the vagus nerve, and alters our gut bacteria. This is because the sympathetic nervous system, our fight or flight response, is activated when we are stressed and prioritizes helping us to flee perceived dangers rather than digest food.
Why do these bacteria cause problems?
- Bacteria produce toxic by-products that damage the microvilli, the absorptive surface of the small intestine, reducing enzymes such as lactase and DAO (diamine oxidase), which can lead to the malabsorption of nutrients, nutrient deficiencies, histamine, and lactose intolerance. When the microvilli are damaged, and not able to digest small starch molecules, the bacteria use these for fermentation. Bacterial fermentation produces methane, hydrogen, and hydrogen sulphide gas which is uncomfortable and causes yet more damage.
- A damaged gut lining can lead to increased intestinal permeability, or “leaky gut”, a condition where partially digested food particles and bacterial endotoxins (part of the outer membrane shed by certain bacteria) can escape through gaps in the intestinal wall, cause an immune reaction and trigger systemic inflammation.
- Bacterial endotoxin-derived gut inflammation impairs gut motility and affects the gut bacteria.
- Bacteria break down bile salts in the intestine which are needed for digestion, especially fat digestion. Insufficient bile salts can lead to fat malabsorption and the malabsorption of fat-soluble vitamins (A, D, E, & K). Ironically vitamins A and D are especially important for gut health.
- Bacteria steal nutrients (B12, iron, magnesium, calcium) before your body has a chance to use them which can lead to nutritional deficiencies.
What common conditions are associated with SIBO?
- Ulcerative Colitis 81%
- Coeliac Disease 9-67%
- Type 2 diabetes 8-44%
- Hypothyroidism 54%
- Chronic Fatigue Syndrome 81%
- Fibromyalgia 93%
- Irritable Bowel Syndrome 4-78%
- Liver Cirrhosis 50%
- Rosacea 46% (2)
What are the symptoms of Small Intestinal Bacterial Overgrowth, SIBO?
Check out below the symptoms of SIBO, symptoms of SIBO vs IBS and hydrogen vs methane SIBO symptoms, and hydrogen sulfide SIBO symptoms.
The symptoms of SIBO are similar to other digestive disorders such as IBS (Irritable Bowel Syndrome), lactose intolerance and fructose malabsorption.
The main gastrointestinal symptoms of SIBO include:
- Diarrhoea and constipation (the previous diagnosis of IBS-C, IBS-D and IBS-M is common)
- Bloating (often extreme, especially after meals)
- Burping and flatulence
- Abdominal pain

Other gastrointestinal symptoms include:
- GERD (Gastroesophageal Reflux Disease)
- Malabsorption/malnutrition
- Steatorrhea (fatty stools)
- Symptoms worse with probiotics
- Inability to tolerate high fibre foods including vegetables, broccoli, legumes, lentils, onions, garlic
Other extraintestinal (non-gut) symptoms of SIBO include:
- Brain fog
- Fatigue
- Anxiety
- Anaemia (B12, iron and ferritin deficiency)
- Rosacea
- Body pain
- Restless legs
- Food intolerances
Other symptoms have been associated with a specific type of SIBO where hydrogen sulfide is produced:
- Irritable bladder (Interstitial Cystitis or Bladder Pain Syndrome)
- Peripheral neuropathy
- Light/noise hypersensitivity
- Muscle pain (fibromyalgia)
- Visceral pain
- Sulphur containing food sensitivity
- Sulphur-smelling flatulence
How do you know if you have IBS or SIBO?
Symptoms of SIBO vs IBS
SIBO is one of the most common causes of inflammatory bowel disease, IBS with some studies suggesting it may affect up to 78% of IBS sufferers (3). Symptoms of SIBO vs IBS are usually indistinguishable.
Comparing the symptoms of SIBO vs IBS, IBS patients have significant effects on their mental health including anxiety and sleep disruptions, SIBO is associated with brain fog. Symptoms of SIBO vs IBS may also overlap. IBS patients, owing to gut microbiome dysbiosis, have increased intestinal permeability and chronic inflammation. It is difficult to distinguish the symptoms of IBS vs SIBO as there are several common and shared symptoms of IBS and SIBO including abdominal pain, distention, diarrhea, and bloating.
It is important therefore to get tested to make sure that you get the correct diagnosis, especially if you have been following a protocol for IBS and it is not working.
What is the difference between hydrogen vs methane SIBO symptoms?
Now we have compared symptoms of SIBO vs IBS, how do hydrogen vs methane SIBO symptoms compare?
As science and testing for SIBO have developed, doctors have recognized the need to differentiate methane SIBO from the more common hydrogen SIBO. This is because it is methanogens, part of the archaea species, that produce methane, not bacteria (the B in SIBO) and they can overgrow in the large intestine, not just the small intestine (the SI in SIBO). They have even proposed a new term for methane SIBO: IMO or Intestinal Methanogen Overgrowth.
When you eat fiber, bacteria produce hydrogen which is consumed by the archaea and used by them to produce methane. The most commonly known methanogen or methane producer is methanobrevibacter smithii.
If we see hydrogen vs methane SIBO symptoms, methane tends to be associated with constipation, severe bloating and weight gain, and hydrogen with diarrhoea. This is because methane slows down stool transit time and causes the body to gain weight. Helicobacter pylori is also associated with methane SIBO. Thus on the basis of hydrogen vs methane SIBO symptoms and testing, we can distinguish the two conditions.
What is hydrogen sulfide SIBO?
After comparing the symptoms of SIBO vs IBS and hydrogen vs methane SIBO symptoms, let us check out hydrogen sulfide SIBO.
Sulphate Reducing Bacteria (SRB) reduce hydrogen to hydrogen sulfide which can then be oxidized into sulfur. It has been proposed that this type of hydrogen sulfide SIBO could be an adaptive response from the microbiome to deal with sulfur deficiency. Infections such as Helicobacter pylori and Klebsiella pneumoniae also produce hydrogen sulfide SIBO.
Unfortunately, hydrogen sulfide is toxic to the body. It is freely permeable to cells and inhibits a bacterial metabolite called butyrate, which plays an important role in protecting the gut mucosal barrier and modulating intestinal motility, pain sensitivity, and inflammation. It is also toxic to mitochondria, the energy powerhouses of the cell, and can cause mitochondrial dysfunction.
What can you do about SIBO?
Phase 1 - Elimination
Antimicrobials
Rifaximin and Neomycin are the first-line antibiotics prescribed for SIBO. Herbal antimicrobials however have been shown to be just as effective as Rifaximin in one study at eliminating bacteria.
Here is how to treat SIBO naturally:
- Berberine
- Oil of oregano
- Oil of red thyme
- Oil of lemon balm (4)
- Garlic
- Neem
Whatever you use, it is important to rotate antimicrobials in order to avoid resistance.

Biofilm disruptors
Bacteria are protected by a tough, extracellular matrix which can make them difficult to penetrate and kill. Biofilm disruptors such as serrapeptidase help to break down that protective shell and are an important part of a comprehensive SIBO protocol. I like Biocidin by Bio-Botanical Research Inc.
Diet Considerations
Many different low, fermentable carbohydrate diets have been proposed to address SIBO. This is because fermentable carbohydrate is the main food source for bacteria. Thus, one can treat SIBO naturally by following these diets.
- Bi-Phasic Diet (Dr. Nirala Jacobi)
- SIBO Histamine Bi-Phasic Diet (Dr. Nirala Jacobi)
- The SIBO Specific Food Guide (Dr. Alison Siebecker)
- SCD (Specific Carbohydrate Diet)
- Cedars-Sinai Low Fermentation Diet (Dr. Pimental)
- GAPS (Guts and Psychology Syndrome) Diet
- FODMAP (Fermentable Oligosaccharides Disaccharides Monosaccharides and Polyols) (Monash University)
- Elemental Diet
The FODMAPS diet is one of the most researched diets and has been shown to be effective in the treatment of functional gastrointestinal complaints (5). FODMAPs are short-chain carbohydrates or sugars that are poorly absorbed by the small intestine. The FODMAP diet substitutes high FODMAP foods such as dairy, wheat, some fruit and vegetables, beans, and lentils for low FODMAP alternatives thereby starving the bacteria of their food source. It is recommended to only follow the FODMAP diet for 2 to 6 weeks under the supervision of a qualified nutritionist. The diet may not be suitable for someone who is underweight or who has an eating disorder.

However, there has been a move away by some practitioners from very restrictive diets and the “starve to kill” approach. This is because they may lead to the reduction of beneficial bacteria known as bifidobacteria. Instead, there is more of a “feed to kill” approach as bacteria go into survival mode where they do not replicate and are harder to penetrate. In addition, restrictive diets may cause food anxiety in some people when foods are reintroduced.
Digestive Support
Prokinetic literally means “promote movement” and prokinetic agents help support gut motility by increasing and strengthening the MMC contractions. They are best taken at night before fasting. Low dose Naltrexone and low dose erythromycin are commonly prescribed. Most natural alternatives contain the ginger root. I like Pure Encapsulations MotilPro and Iberogast.
Avoiding drinking water when eating a meal is important as this reduces the concentration of stomach acid needed to properly digest your food and absorb nutrients.
Bitter foods help to stimulate the production of bile needed for digestion, especially fats, and gut motility. They include:
- Salad leaves – rocket, radicchio, watercress, and endive
- Herbs – parsley, mint, coriander, and thyme.
- Citrus fruits – lemon, orange, grapefruit
Including them in a salad as a starter with a squeeze of lemon juice or vinegar is an easy way to incorporate them into your diet.
Eating mindfully encourages the body to prepare for ingested food by stimulating the production of stomach acid and digestive enzymes.
Eating whilst relaxed helps to put your body in a parasympathetic state, otherwise known as the “rest and digest” state. This means that the body is able to properly digest.
Digestion begins in the mouth and by chewing properly (30 times per mouthful) you can help the stomach to break down food so that it can be completely absorbed in the small intestine and not be left to feed bacteria.
Meal spacing (leaving at least 4 hours in between meals) allows your MMC (Migrating Motor Complex) to properly digest food and “clean up” any undigested food, particles, and bacteria.
Supplements containing betaine HCL (hydrochloric acid) and digestive enzymes may aid digestion. I like Designs for Health Digestzymes as it combines the two.
Nutritional Support
It may be helpful to supplement fat-soluble vitamins, B vitamins, and iron in the case of nutritional deficiency. Vitamins A and D will also help support gut health.
Stress Management
Stress has an inhibitory effect on digestion therefore lowering stress levels is important. The following stress management techniques may be helpful:
- Breathing techniques (Buteyko, diaphragmatic)
- Meditation
- Low-intensity exercise i.e. Yin yoga
- Good sleep hygiene
- Acupuncture
- Reflexology
Liver Detoxification
Bacterial die-off causes a build-up of toxins in the liver, our main detoxification organ, so it is a good idea to support the liver during eradication. Pure Encapsulations Liver G.I. is a good multi-blend.
Additional Therapies
Many other therapies may be used alongside nutritional therapy and may be helpful:
- Bowen Technique
- DNRS (Dynamic Neural Retraining System) by Annie Hopper
- VNS (Vagus Nerve Stimulation)
- Osteopathy/chiropractor/physiotherapy
- Biofeedback therapy
Phase 2 - Relapse Prevention
Microbiome support
After successful eradication of bacterial overgrowth and remediation of symptoms, it is important to rebalance the gut with beneficial bacteria and to heal the gut lining. This may seem counterintuitive but good bacteria is crucial to our overall health.
Probiotics are the friendly or “good” bacteria in your gut and have been proven to be effective in the treatment of SIBO (6). Using a high CFU (Colony Forming Units) lactobacillus and bifidobacterial blend, saccharomyces boulardii, and soil-based probiotics, such as bacillus, is a good strategy. However, there is no “one size fits all” as different strains and combinations are tolerated differently. Probiotics foods such as kefir, sauerkraut, and miso may be gradually introduced.
Prebiotics feed friendly bacteria so are also important. Prebiotic foods include chicory root, leeks, garlic, onion, and Jerusalem artichoke. PHGG (Partially hydrolyzed guar gum) and GOS (galacto-oligosaccharides) are generally well tolerated and shown to reduce methane.
Postbiotics have been getting a lot of press recently. They are the bioactive compounds such as SCFA (Short Chain Fatty Acids) that the probiotic bacteria produce when they consume the prebiotics and may also help to support gut health.
Gut Healing
There are many dietary and supplement recommendations for reducing gut inflammation and promoting healing:
- Fish oil (EPA – eicosapentaenoic acid)
- Slippery elm
- Marshmallow root
- L-glutamine
Phase 3 – Treat the Underlying Causes
Relapse rates are high. In order to extend remission and avoid relapse the most important part of the protocol is to address the underlying causes as outlined earlier. It may be necessary, for example, to test for chemical toxins or mycotoxins if you have completed a SIBO protocol but are still having gut symptoms.
Should you re-test for SIBO?
Yes, re-testing is important in order to assess how well the treatment is working and to provide some encouragement for the patient. Some practitioners test after antimicrobial therapy, and some at the end of the program.
The Final Words
I hope this article has helped you to understand SIBO a bit better and has encouraged you to seek help if you are experiencing some of the symptoms of SIBO vs IBS, hydrogen vs methane SIBO, and hydrogen sulfide SIBO I have discussed. Healing Small Intestinal Bacterial Overgrowth or SIBO is not a quick fix but with time and dedication, it is possible to get rid of it.
Sources
- Dukowicz AC Lacey BE Levine GM. Small Intestinal Bacterial Overgrowth: a comprehensive review. Gastroenterol Hepatol (NY). 2007 Feb. 3(2): 112-122. Available from: https://pubmed.ncbi.nlm.nih.gov/21960820/
- Grace E Shaw C Whelan K Andreyev HJN. Review article: Small Intestinal Bacterial Overgrowth- – prevalence, clinical features, current and developing diagnostic tests, and treatment. Alliment Pharmacol Ther. 2013 Oct. 38(7):674-88> Available at: https://pubmed.ncbi.nlm.nih.gov/23957651/
- Ghoshal UC Shukla R Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: a bridge between the functional organic dichotomy. Gut Liver. 2017 Mar. 11(2):196-208. Available from: https://pubmed.ncbi.nlm.nih.gov/28274108/
- Chedid V Dhalla S Clarke JO Roland BC Dunbar KB Koh J et al. Herbal therapy is equivalent to Rifaximin for the treatment of Small Intestinal Bacterial Overgrowth. 2014 May. 3(3):16-24. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4030608/
- Tuck CJ Vanner SJ. Neurogastroenterol Motil. 2018 Jan. 30(1). Available at: https://pubmed.ncbi.nlm.nih.gov/29094792/
- Khalighi AR Khalighi MR Behdani R Jamali J Khosravi A Kouestani Sh et al. Evaluating the efficacy of probiotics on treatment in patients with Small Intestinal Bacterial Overgrowth (SIBO) – a pilot study. Indian J Med. Res.2014 Nov. 140(5):604-8. Available at: https://pubmed.ncbi.nlm.nih.gov/25579140/

Lucy Owens
Related Posts

Ka’Chava Reviews, Ingredients, Side Effects: Elevate Your Nutrition With Superfood Shakes

Provitalize Reviews, Ingredients, Side Effects – Does This Thermogenic Probiotic Work?